Cardiac Ultrasound
Indications
- Assessment of the presence of pericardial effusion
- Assessment of global cardiac systolic function
- Identification of marked RV/LV enlargement
- Intravascular volume status
- Guidance of pericardiocentesis
- Confirmation of transvenous pacing wire placement
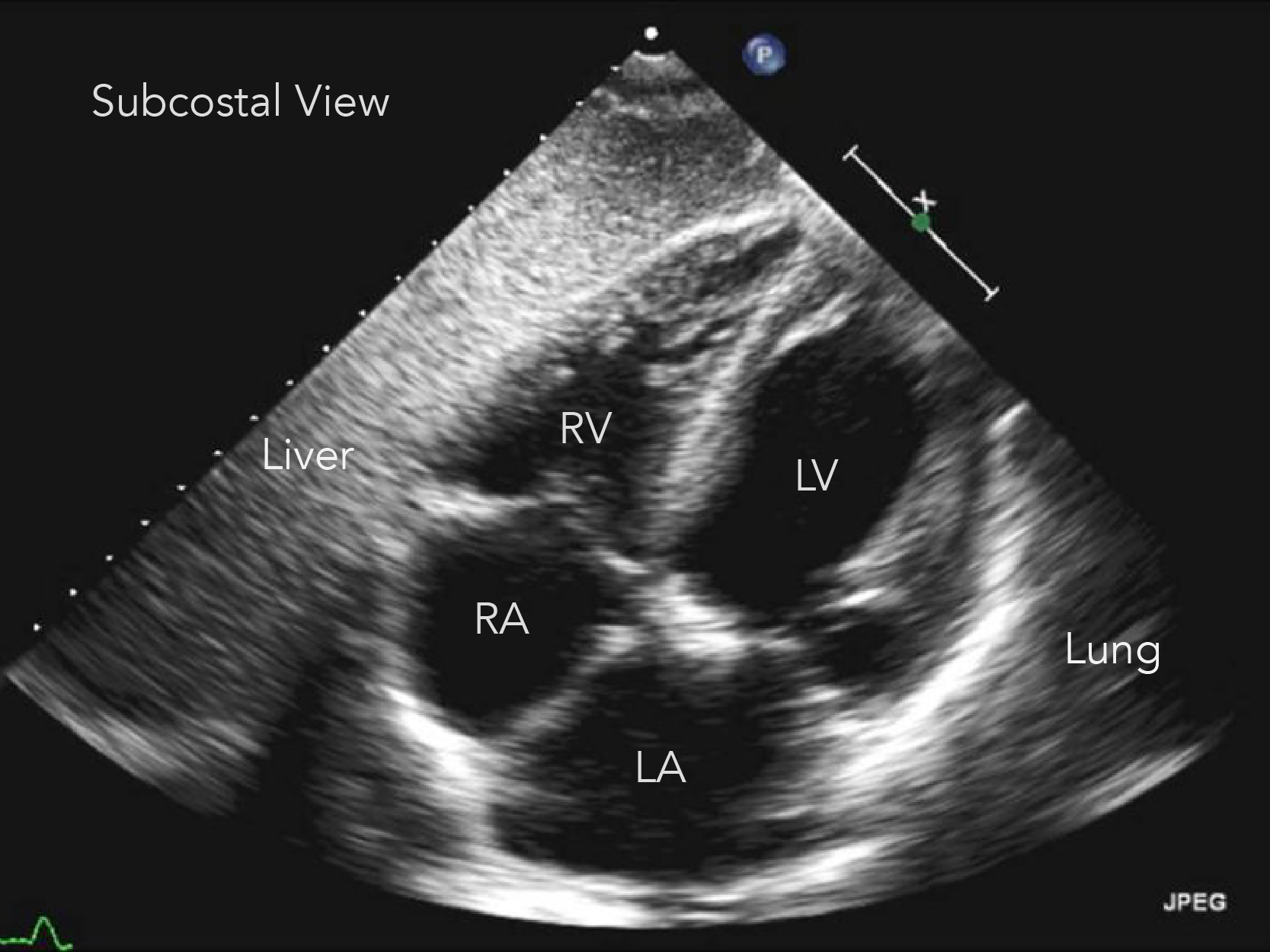
Key Ultrasound Anatomy
Documentation
Cardiac ultrasound should include representative image or clip from each of the following windows:
- Subxiphoid/Subcostal
- Parasternal Long Axis
- Parasternal Short Axis
- Apical
Approach
A cardiac exam for pericardial effusion and cardiac function/activity should include adequate views of the heart including anterior and posterior pericardium and should include the following windows: Subxiphoid/Subcostal, Parasternal Long Axis, Parasternal Short Axis, Apical
Probe and Positioning
- 2-5 MHz curvilinear abdominal probe or smaller footprint curved array or phased array probe
- Patient is supine or in left lateral decubitus position.
Clinical Question & Exam interpretation
- Is there a pericardial effusion?
- Any pericardial fluid should be considered a positive scan and either direct further care or be followed up with confirmatory ECHO.
- Is the LV systolic function normal?
- Assess LV contractility and determine if it is normal or reduced (mild, moderate, severe).
- Is there cardiac activity?
- Evaluation of cardiac activity should be performed simultaneously with appropriate resuscitative interventions.
Pearls & Pitfalls
- The subcostal window is ideal for assessing a pericardial effusion and assessing for signs of tamponade. Often bowel gas may obstruct your view, attempt to slide probe more towards the patient's right side, directed at their left shoulder to use the liver as a better acoustic window
- Often you will be unable to obtain a particular view in a patient due to body habitus or underlying cardiopulmonary disease. Before giving up first try changing position, such as sitting the patient up to 30 degrees or placing them in the left lateral decubitus position. The apical view should always be obtained in the left lateral decubitus.
- An ideal parasternal long axis view will display the LV outflow tract running approximately perpendicular to your probe with the RVOT,LVOT and LA in the midline of your image. You should visualize both the mitral valve and the aortic valve to know that you are not off axis.
- In a normal parasternal long axis, the RVOT, aorta and LA should all take up approximately 1/3 of the screen. Any difference in this ratio should raise concern for pathology.
- You should always obtain a minimum of 3 parasternal short axis views: At the level of the aortic valve, at the level of the mitral valve, and at the level of the papillary muscles (mid-ventricle). The left ventricle should lie in the middle of the screen and appear round and symmetric for this to be an adequate view.
- In the apical 4 chamber view, it may be difficult to distinguish the LV from the RV with pulmonary pathology such as pulmonary embolism or pulmonary hypertension. Be sure to always use the same prober marker orientation when performing this view to avoid this. If you are still unsure, you can use the AV valves to determine which chamber is which. The mitral valve will attach to the septum more distal from the apex of the heart that the tricuspid valve.
FOAMed Curriculum
- Emergency Echo at Emergency Ultrasound Teaching
- Effusions & Tamponade at Ultrasound Village
- SAEM Echo Lectures Part 1 Part 2
- Ultrasound Guided CPR at Ultrasound Podcast
- SAEM IVC Volume Assessment