Written by: Daniel Levine, MD (NUEM ‘23) Edited by: Will LaPlant, MD, MPH (NUEM '20) Expert Commentary by: Matt Levine, MD
Expert Commentary
Thank you for the handy concise reference for felon management. Some key points of emphasis and elaboration:
A TENSE distal finger pad is what distinguishes a felon from other finger infections. A paronychia can be the portal of entry (as in this case https://www.ortho-teaching.feinberg.northwestern.edu/cases/hand/case14/index.html) . However, a paronychia alone should not cause a TENSE finger pad so check the finger pad before diagnosing a finger infection as a simply a paronychia. Flexor tenosynovitis is not localized to the distal pad and should be readily distinguishable from a felon, which is localized. Whitlow may be confused for a purulent infection but is cutaneous and again, will not have a TENSE pad.
The felon itself is an intense throbbing pain and the procedure is extensive so analgesia is a major point of emphasis for successful management.
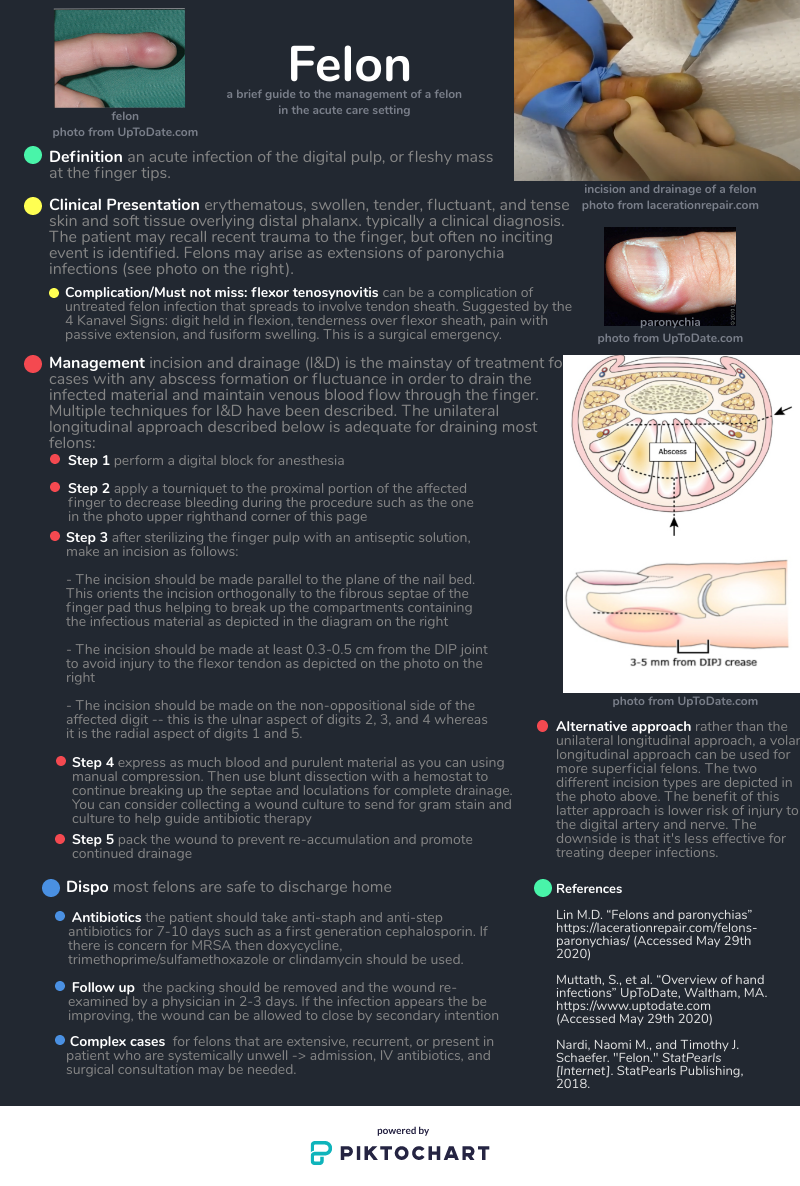
The key to understanding the nature and treatment of a felon is knowledge of the anatomy of the distal finger. There are 15-20 discrete, noncompliant, tough fibrous septae of the finger pad which run from the periosteum to the skin. The abscess of a felon affects these unforgiving septae, which is why is it so painful. The incision must enter the septae and the dissection must break up the remaining septae to completely drain the infection. Other abscesses we drain may have loculations but not the tough septations of a felon. So the dissection must be firm enough to break these septations.
There are many different (and interestingly named) incisions that have been described to decompress a felon, like the “hockey stick” (https://lacerationrepair.com/felon-hockey-stick/) or the “fish mouth” (https://lacerationrepair.com/felon-fish-mouth/). Many sources prefer lateral approaches over volar approaches. The volar approaches incise directly through the highly innervated pad and residual paresthesia affecting finger function is a concern.
Be aware that you are dissecting just volar to the phalanx to get into these septae, so this is deep. If the etiology of the felon is direct extension from a paronychia, drain the paronychia first and see if you can access the felon by dissecting through the paronychia tract. Afterwards, insert packing or a drain. I have even seen consultants make bilateral incisions and feed a drain all the way through to facilitate drainage.
Refer all of these patients to hand clinic. One patient I had who was lost to follow up returned to the ED weeks later with osteomyelitis of the distal phalanx (https://www.ortho-teaching.feinberg.northwestern.edu/cases/bone-lesions/case4/index.html).
Matthew R Levine, MD
Associate Professor of Emergency Medicine
Northwestern Memorial Hospital
How To Cite This Post:
[Peer-Reviewed, Web Publication] Levine, D. LaPlant, W. (2021, March 8). Felon. [NUEM Blog. Expert Commentary by Levine, M]. Retrieved from http://www.nuemblog.com/blog/felon.