Written by: Patricia Bigach MD, (NUEM ‘23) Edited by: Terese Whipple (NUEM ‘20) Expert Commentary by: Seth Trueger MD, MPH
Expert Commentary
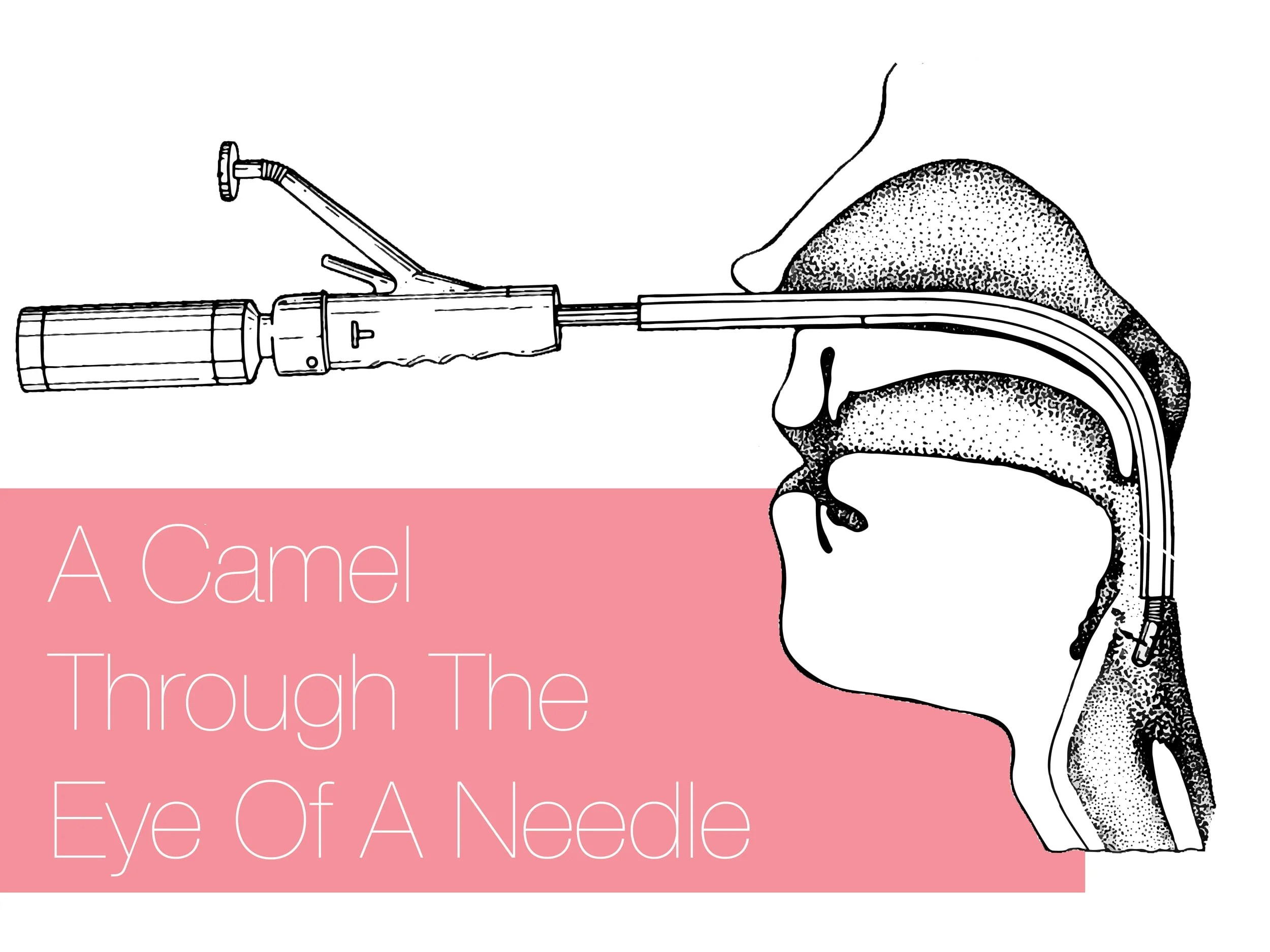
Awake intubation can sound imposing but simply means the patient is still breathing on their own. It is mostly just a matter of using topical lidocaine instead of paralyzing, and sedating the patient a bit to tolerate it. It will almost always require some sedation – ketamine procedural sedation works very well as the patient’s protective reflexes will be intact (until we topicalize) as will their respiratory drive.
It does not take long! Just spray lido instead of pushing NMBA. This is the key concept. If time is really a factor, I atomize the larynx, push ketamine, and then reload and spray more lidocaine as I do laryngoscopy; everything else is just like every other ED intubation.
Glycopyrrolate is nice but if it’s not handy, not worth a delay.
I find nebulizing doesn’t add much, mostly just gets the mouth. I still nebulize if I can get it set up quickly while prepping everything else (and it can help tolerate the atomizer).
Small touches of propofol might help relax the ketamine-sedated patient as well, including spontaneous/dissociated movements and tightly closed mouths. Dexmedetomidine might not be fast enough for ED intubations.
I usually use hyperangulated VL (eg Glidescope S3) – we are usually doing this for predicted difficult intubation, and now not optimizing intubating conditions. Fiberoptic requires a fair amount of skill and time. One of the main things that demystified awake intubation for me is it is a medication choice; it doesn’t always mean awake-fiber optic.
In non-COVID times, I would keep the nasal cannula on at 5-15lpm to keep the patient as oxygenated as possible, which is even better than during RSI because they’re still breathing, now with extra oxygen.
The paradox of awake intubation is that we take the patients we predict to be the most difficult anatomically, and then don’t optimize intubating conditions (no NMBA). Part of the beauty of awake intubation is that we also gain a ton of information even if unsuccessful without losing much; if I get a partial view in non-NMBA circumstances I can make a judgment call about proceeding to paralysis (ie RSI) or calling for help, etc.
Sedation-only or ketamine-only intubation can sound like a good idea but neither makes sense to me. It takes a lot of sedation to knock out protective airway reflexes to allow laryngoscopy, i.e. enough to impair respiratory drive. Topicalization is not hard with atomizers. Similarly, ketamine keeps the airway reflexes intact, which is why it is so safe for procedural sedation, so hard to imagine that laryngoscopy won’t be an issue.
Seth Trueger, MD, MPH
Assistant Professor of Emergency Medicine
Department of Emergency Medicine
Northwestern University
How To Cite This Post:
[Peer-Reviewed, Web Publication] Bigach, P. Whipple, T. (2021, Aug 20). Awake Intubation. [NUEM Blog. Expert Commentary by Trueger, S]. Retrieved from http://www.nuemblog.com/blog/awake-intubation