Written by: Katie Colton, MD (NUEM PGY-4) Edited by: Charles Caffrey, MD (NUEM Alum ‘18) Expert commentary by: Andrew Pirotte, MD
The patient
On a recent Thursday night in a single-attending ED, we received a call that a patient was several minutes out with respiratory distress. He had been enjoying his routine post-dinner cocaine insufflation and became dyspneic, per bystanders. We could hear yelling in the back of the ambulance and EMS reported that they were only able to get an oxygen saturation, which was about 70%.
The scene
Two minutes later, EMS rushed in with a patient who looked to be in his mid-50s who was clearly struggling to breathe; it required 6 people to transfer him to our cart. He was altered, hypoxic, approximately 500 pounds, and needing an airway in the near future. While there are many considerations for the difficult airway, what are particular positioning options that may increase the chances of success in this patient?
“Positioning is 90% of the battle”
Beyond the technical difficulties posed by the morbidly obese patient, there are physiologic differences that complicate their oxygenation and ventilation. Due to the weight of the chest and larger abdomen they will have a decreased functional residual capacity and total lung capacity. Supine position can complicate pre-oxygenation, endotracheal intubation (ETI), and cause hypotension in these patients.
Many providers are still trained almost entirely in ETI with a supine patient, but there is growing evidence that a head-up position can improve pre-oxygenation and facilitate ETI.
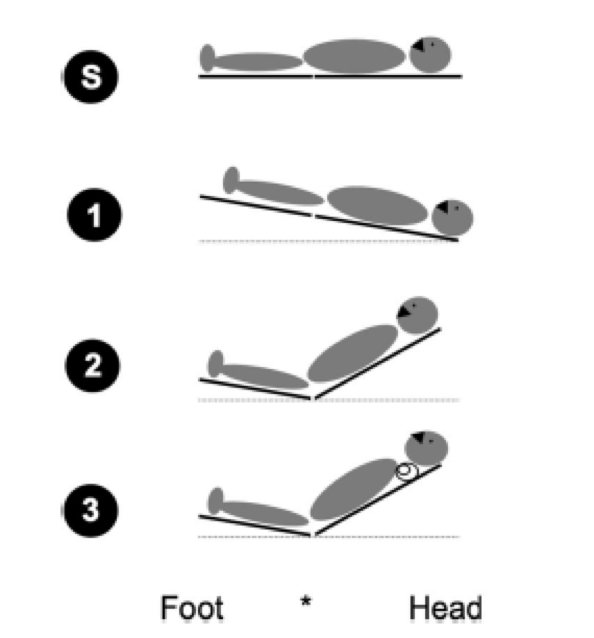
Some authors advocate for an aggressive ramped position, using either a pre-formed foam ramp or a stack of pillows or blankets, like in the pictures below. I would argue that unless you have a stack of pillows at the ready and a number of spare hands this technique may be difficult in the less-controlled setting.
(Simoni 2005)
So then what?
Newer studies – and anecdotal experience - are showing good results with upright intubation through simple manipulation of the head of the bed. One example of this is the back-up head-elevated position as seen below[2]. First, by brief placement of the patient into Trendelenburg, the patient is brought all the way to the top of the bed (1 in image), and then the back of the bed is ramped up to at least 30 degrees above the horizontal (2 in image), with the head placed into the “sniffing” position with a towel roll (3 in image).[2] In their retrospective analysis, Khandelwal et al. found a lower rate of intubation-related complications as compared to a supine cohort, 9.3% vs 22.6%.[2]
(Khandewal 2016)
How to place the patient in the advised back-up, head-elevated position.
A team from IU showed improved intubation success with head of bed elevation in both a simulated [4] and ED setting [3]. This approach allows the patient to be positioned during preoxygenation. Redundant tissue falls away from the face and chest, improving the patients ability to breathe for themselves and the ease of BVM, if needed. Khandelwal et al found lower risk of aspiration and esophageal tube placement. For every 5 degree increase in head of bed angulation above the horizontal, Turner et al found increased likelihood of first pass success with ETI.
(Turner 2017)
In short, consider using the bed to your advantage in these difficult patients. It takes time to overcome habits but there is good evidence for changing up your positioning plan.
Case Conclusion
The patient’s head of the bed was ramped up to 45 degrees. Utilizing rapid sequence intubation, the resident took one look with a size 4 Macintosh acquiring a Grade II view, and was able to place an 8-0 tube. A follow-up chest x-ray showed appropriate placement and frank pulmonary edema. The patient was treated for pulmonary edema and admitted to the ICU.
Expert Commentary
As with all clinical excellence, the devil is in the details. Skillful airway management requires attention to detail, notably patient positioning. This case and review serve as a reminder that close attention to setup and positioning can help enhance successful airway management.
Positioning is critical to airway success. Particularly in the setting of higher body-mass index patients, optimized positioning is a critical step to safe and successful airway management. As suggested by the review, simply placing the patient in supine positioning is not optimal and should be avoided if possible. Improved positioning can be achieved in several ways, but often the most straight-forward is by raising the head of the bed, or stacking towels and pillows. This position is often referred to as the “sniffing” position.
The sniffing position refers to bringing the sternal notch and the ear into the same plain (see blog post image). This positioning not only improves ergonomics for the clinician, but provides enhanced laryngoscopy and endotracheal tube delivery success. In addition, sniffing positioning compliments and enhances other airway optimization strategies.
One significant benefit of the sniffing position is preventing collapse of soft tissue and occlusion of the airway. The relief of redundant tissue with the sniffing position likely improves high-quality mask ventilation, as the tissue collapse into the posterior oropharynx is less prominent. Physiological benefits of sniffing position also include decreased lung atelectasis and improved delivery of oxygen during airway preparation. Considering these points, utilization of the sniffing position (rather than supine positioning), vitally strengthens the airway management pathway.
Positioning remains crucial to optimized airway delivery. The sniffing position does not require expensive equipment or great skill; it is a straight-forward, useful, and impactful strategy to enhance airway management. As emergency airway management continues to evolve, much focus has been on enhancing laryngoscopy. In addition, there have been great strides in technology and monitoring equipment. But even with the best equipment and technology, simple strategies such as optimizing positioning can lead to high-yield results.
Special thanks to Dr. Jordan Kaylor and Dr. Matthew Pirotte
Andrew Pirotte, MD
Department of Emergency Medicine, University of Kansas Hospital
Clinical Assistant Professor, University of Kansas Medical Center
How to Cite This Post
[Peer-Reviewed, Web Publication] Colton K, Caffrey C (2019, February 4). Intubation Positioning: Beyond Sniffing [NUEM Blog. Expert Commentary by Pirotte A]. Retrieved from http://www.nuemblog.com/blog/intubation-positioning.
Other Posts You May Enjoy
Resources
RF Simoni et al. Tracheal Intubation of Morbidly Obese Patients: A Useful Device. Brazilian Journal of Anesthesiology, 2005; 55: 2: 256-260
N Khandelwal et al. Head-Elevated Patient Positioning Decreases Complications of Emergent Tracheal Intubation in the Ward and Intensive Care Unit. Anesth Analg. 2016 Apr;122(4):1101-7.
Turner JS et al. Feasibility of upright patient positioning and intubation success rates at two academic emergency departments. Am J Emerg Med. 2017 Feb 5. pii: S0735-6757(17)30100-6.
Turner JS et al. Cross-over study of novice intubators performing endotracheal intubation in an upright versus supine position. Intern Emerg Med. 2016 Jun 14.