Written by: Emmanuel Ogele, MD (Cook County Stroger PGY-1) Edited by: Spenser Lang, MD (NUEM Alum '18) Expert commentary by: James Walter, MD
ABG’s vs VBG’s in the Emergency Department
Arterial blood gases (ABG’s) – blood sample taken directly from an artery used to gauge the metabolic environment, oxygenation, and ventilation status. Values such as pH, PCO2, PaO2, HCO3, and Base Excess obtained via ABG are considered the gold standard.
Venous Blood gases (VBG’s) – blood sample taken from either peripheral or central veins –can serve as an alternative to an ABG when evaluating patients with metabolic and respiratory disturbances.
Historically, values obtained via VBG have been criticized for a perceived lack of accuracy in all domains.
However, VBGs carry less risk of vascular injury, nerve damage, and cause much less pain to the patient along with lower risk for accidental needle-sticks as compared to ABGs
So the question remains – are values (such as pH, PCO2, and HCO3) truly disparate enough between ABG’s and VBG’s to actually change clinical practice?
Increasing data shows that for most clinical indications, data from VBG correlates well, and are just as useful as that from ABG.[1-4]
Zeserson et. al. conducted a prospective cohort study of 156 critically ill patients in the ED and ICU setting to evaluate the correlation between pH and pCO2 when derived from ABG vs VBG with added pulse oximetry for estimating PaO2 and concluded that arterial and venous pH and PCO2 had good correlation.
Byrne et al conducted a meta – analysis of 1768 subjects from 18 individual studies and found that peripheral VBG correlates well with ABG with respect to pH but found an unacceptably wide 95% prediction interval when looking at the pCO2.
A review article by Kelly AM summarized data comparing ABG and peripheral VBG variables in ED all-comers also concluded that venous pH had sufficient agreement however concluded with a word of caution: there is no data to support that this correlation is maintained in shock states.
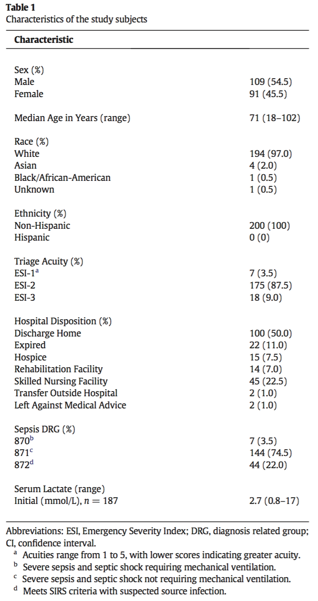
Several studies have looked at the correlation between values obtained with VBG and compared them to ABG. These are summarized in Table 1.
Table 1. Correlation of VBG to ABG values
** Widest limit of agreement from any single study included in the meta-analysis
For most parameters, there is good correlation. However, there are a few important scenarios that may be exceptions. Not surprisingly, the major exception is PO2; venous PO2 readings do not correlate well with arterial PO2. A workaround to this limitation is to estimate arterial oxygenation using SpO2.
The VBG analysis plus SpO2 provided accurate information on acid–base, ventilation, and oxygenation status for patients in undifferentiated patients ED and ICU.[2]
VBGs are acceptable to use in working up common conditions like COPD and DKA.[5,6] New data could potentially broaden the list of indications for VBG instead of ABG
Ma OJ et al. conducted a prospective trial looking at the utility of ABG in patients presenting to the ED with suspected DKA and found that ABG analysis changed management of DKA 1% of the time and concluded that VBGs are a viable substitute.
Conditions that may affect the reliability of VBG
Hypercapnia.
When comparing VBG and ABGs, the average difference in CO2 reading was 5.7 mmHg. [1]
However, the limits of agreement (-17.4 to +23.9) in this study are too wide to allow reliable quantification of PCO2.
In sum, if you need a precise PCO2 number for clinical decision making, a traditional ABG is preferable.
One such scenario where a true PCO2 can be useful is evaluating for acute hypercapneic respiratory failure; however, a VBG still has some utility.
In the prospective study by AM Kelly 7 a PCO2 value above 45mmHg had a 100% sensitivity for true hypercapnia. This makes a VBG PCO2 value useful in screening for hypercapnia. 5
Shock Pearls
VBGs show increased discordance from ABGs in hypotensive patients.[8]
pH and PCO2 values may be wildly disparate in patients with severe circulatory failure.[9]
In sum, venous blood gases may be increasingly inconsistent with arterial blood gases in patients with increasing degrees of shock. No definitive data exists yet to tell us if VBGs are sufficient to replace ABGs in shock states.
Mixed Acid Base Disorders
There is insufficient evidence to confirm reliability of VBGs in these cases
In summary, VBGs can be used as a reliable alternative to ABGs in many clinical cases. The patients’ benefits of a VBG vs ABG are obvious – decreased pain, complications, and time. Clinical judgment must be used in deciding when to the substitute a VBG for a more traditional ABG. The evidence is mixed, and even non-existent in some clinical scenarios. In the future, noninvasive methods of evaluation, such as transcutaneous PCO2 monitoring and ETCO2, could allow for accurate for non-invasive and monitoring of the metabolic milieu.
Expert Commentary
ABGs vs VBGs in the Emergency Department: Expert Commentary
Thank you for the opportunity to share some thoughts on this topic. The ABG vs VBG debate has been the source of a lot of discussion and at times disagreement between EM and IM. I am hopeful that we are starting to reach consensus on their respective advantages, disadvantages, and indications. When deciding on which test to obtain, here are a few questions to ask yourself:
1. What is my clinical question?
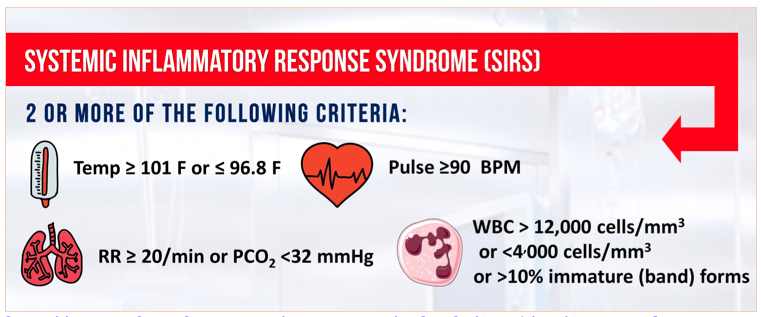
Diagnostic tests should be performed to answer a specific clinical question. Defining this question will help ensure you order the correct test, or perhaps appropriately order no test at all. For blood gas sampling this question might be: “Does my patient with a COPD exacerbation have significant hypercapnia?”; “Is my patient appropriately compensating for his metabolic acidosis?”; “Is my hyperglycemic patient acidotic?” If you can’t articulate a specific question, or if the answer to that question is unlikely to change your management (i.e., a question of “is my patient acidotic?” for a 70-year-old with urosepsis whose blood pressure has responded to 1L of fluid and looks well), then you can probably save your patient an unnecessary blood draw and avoid blood gas sampling altogether. This is certainly an issue for us in the ICU. Patients with arterial lines will have standing Q6hr ABG orders for 2 days before anyone asks if those blood draws are actually changing our management. Don’t order an ABG or VBG just because a patient has sepsis, or they have COPD, or you are “screening for badness.” Using a POC or rapid VBG with a metabolic profile to rapidly obtain lab values for patients presenting to the ER is reasonable. Outside of this situation, try to make sure you are asking a specific question and that answering that question is likely to change what you do.
2. Am I screening for hypercapnia?
If your clinical question is, “is my patient hypercapnic?” then a VBG is a great test. As noted above, a PvCO2 < 40 mmHg excludes hypercapnia. This can be an extremely helpful in the rapid workup of altered mental status and many other common presenting conditions.
3. How accurate do I need my PCO2 value to be?
If the answer to this question is “not that accurate” then a VBG is probably fine. Having a rough estimate of PCO2 levels is usually adequate for the management of mild-moderate DKA, COPD exacerbations, and many other conditions managed in the ED. While a PvCO2 value of 18 mmHg or 75 mmHg may not exactly correlate with what you find on a PaCO2, they are abnormal enough to give you a good general sense of things.
If you are interested in performing a more refined blood gas analysis such as determining the chronicity of a respiratory acidosis, measuring shunt fraction, or accurately quantifying a hypercapnic patient’s true PCO2 then you probably need an ABG. As noted above, the correlation between PaCO2 and PvCO2 is often poor.
4. Am I assessing oxygenation?
At times, obtaining a reliable SpO2 can challenging especially in patients with PAD, scleroderma, or shock. If you need an accurate assessment of oxygenation then you need an ABG. PvO2 values do not correlate well at all with PaO2.
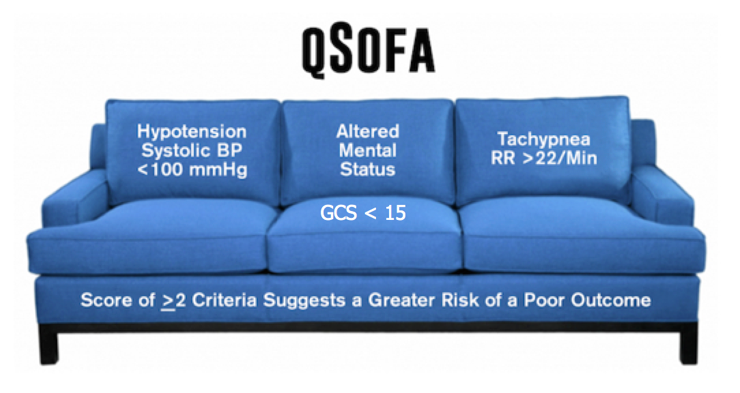
5. Is my patient in shock?
As noted above, VBGs are much less accurate in shock. Unfortunately, this is where we are often most interested in frequent blood gas analysis. In the ED, I think ABGs are most useful (and underused) in critically ill acidotic patients who may or may not have appropriate respiratory compensation. This determination is hard to make on clinical grounds alone (i.e. the signs of early respiratory muscle fatigue can be subtle) and identifying fatigue may well change your management (pushing you to earlier NIV or mechanical ventilation). I would hesitate to solely rely on VBGs in this setting especially for patients in overt shock.
A few other points:
I do think the risks of an ABG as stated above and in other reviews (for example, https://lifeinthefastlane.com/ccc/vbg-versus-abg/) are overstated. A competent clinician should be able to obtain an ABG from a radial artery in a matter of seconds. If there are any concerns regarding anatomy or first stick accuracy, the use of a vascular ultrasound probe can remove any guess work from finding the best arterial access site. ABGs do require an extra needle stick for patients so clinicians should be discerning about their use. However, if one is indicated they shouldn’t be avoided for fear of causing a pseudoaneurysm or major bleeding. Compared to innumerable other invasive procedures and diagnostic tests performed in the ED, ABGs are pretty benign. For some reason, they are still frequently described like thoracotomies.
Remember the following rough corrections
Venous pH is 0.03 lower than arterial pH (venous pH 7.27 = arterial pH 7.3)
Venous PCO2 is 6 mmHg higher than arterial PCO2, but with wide variability; in general, difficult to predict arterial PCO2 from venous PCO2 (although a PCO2 can still be useful, as noted above).
James Walter, MD
Pulmonary and Critical Care, Northwestern Medicine
Medical Director of the Northwestern Lung Rescue Program
How to Cite This Post
[Peer-Reviewed, Web Publication] Ogele E, Lang S (2018, October 15). VBG vs ABG in the ED. [NUEM Blog. Expert Commentary by Walter J]. Retrieved from http://www.nuemblog.com/blog/vbg-abg
Other Posts You May Enjoy
Resources
Kelly AM. Review article: Can venous blood gas analysis replace arterial in emergency medical care? Emerg Med Australas. 2010 Dec;22(6):493-8. doi: 10.1111/j.1742 6723.2010.01344.x. Review. PubMed PMID: 21143397
Zeserson E, Goodgame B, Hess JD, Schultz K, Hoon C, Lamb K, Maheshwari V,Johnson S, Papas M, Reed J, Breyer M. Correlation of Venous Blood Gas and Pulse Oximetry With Arterial Blood Gas in the Undifferentiated Critically Ill Patient. J Intensive Care Med. 2016 Jun 9.
Byrne, A. L., Bennett, M., Chatterji, R., Symons, R., Pace, N. L. and Thomas, P. S. (2014), Peripheral venous and arterial blood gas analysis in adults: are they comparable? A systematic review and meta-analysis. Respirology, 19: 168–175. doi:10.1111/resp.12225
Kelly AM, McAlpine R, Kyle E. Venous pH can safely replace arterial pH in the initial evaluation of patients in the emergency department. Emerg Med J. 2001
McCanny, Venous vs arterial blood gases in the assessment of patients presenting with an exacerbation of chronic obstructive pulmonary disease.
Ma OJ, Rush MD, Godfrey MM, Gaddis G. Arterial blood gas results rarely influence emergency physician management of patients with suspected diabetic ketoacidosis. Acad Emerg Med. 2003 Aug;10(8):836-41. PMID 12896883
Anne-Maree Kelly, Elizabeth Kyle, Ross McAlpine, Venous pCO2 and pH can be used to screen for significant hypercarbia in emergency patients with acute respiratory disease, In The Journal of Emergency Medicine, Volume 22, Issue 1, 2002, Pages 15-19, ISSN 0736-4679, https://doi.org/10.1016/S0736-4679(01)00431-0.
Shirani F, Salehi R, Naini AE, Azizkhani R, Gholamrezaei A. The effects of hypotension on differences between the results of simultaneous venous and arterial blood gas analysis. Journal of Research in Medical Sciences : The Official Journal of Isfahan University of Medical Sciences. 2011;16(2):188-194
Adrogué HJ, Rashad MN, Gorin AB, Yacoub J, Madias NE. Assessing acid-base status in circulatory failure. Differences between arterial and central venous blood. N Engl J Med. 1989 May 18;320(20):1312-6.




























































































![Figure 2. Left Lateral Decubitus Film [9]Left lung collapses when in dependent position. This is normal and does not suggest foreign body or air trapping in left lung.](https://images.squarespace-cdn.com/content/v1/549b0d5fe4b031a76584e558/1532104060396-YKC9XJE1PAZLQFSY8M58/Picture1.png)
![Figure 3. Right Lateral Decubitus Film [9]Right lung does not collapse when in dependent position. This is abnormal and suggests foreign body in right bronchus causing air trapping in right lung.](https://images.squarespace-cdn.com/content/v1/549b0d5fe4b031a76584e558/1532104241725-LTBFSCB9AM35GBMQ3CX5/Picture2.png)