Written by: William Ford, MD, MBA (NUEM PGY-2) Edited by: Allison Marshall, MD (NUEM 2017 Graduate) Expert Commentary by: Luke Rosier, MD
The Case
A 64-year- old male with diabetes, hypertension, hyperlipidemia and kidney stones presented with 2 hours of acute onset epigastric and left flank pain. As paramedics wheeled him to a room, the patient was clutching his abdomen, wailing in agony, with vital signs notable for a blood pressure of 204/96 mmHg and tachycardia. Being that the patient appeared in acute distress and you had several life threatening diagnoses on your differential, a bedside ultrasound was performed and the following images were obtained:
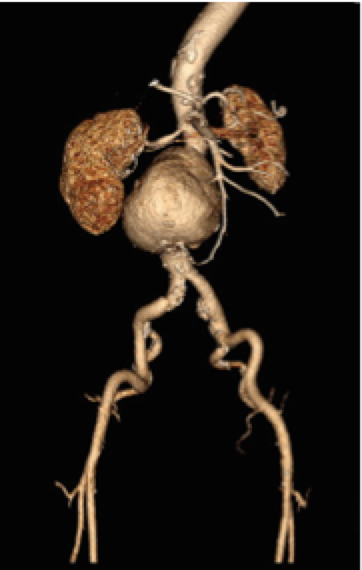
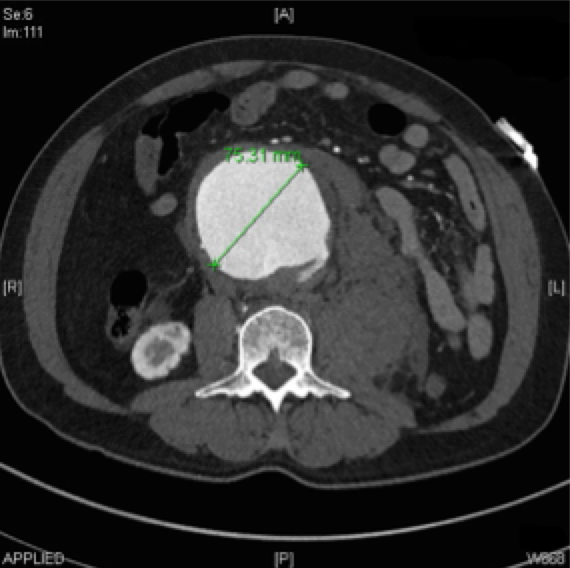
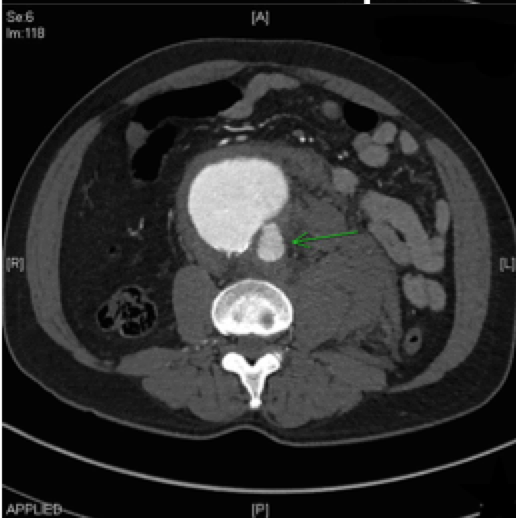
Vascular surgery was emergently consulted for this symptomatic abdominal aortic aneurysm (AAA) and the patient was taken for CT. An esmolol drip was started to reduce aortic wall stress in the context of his hypertension and tachycardia.
A Silent Killer
Around 30% of symptomatic AAAs are misattributed to non-vascular causes leading to poor outcomes [5]. The classic triad of abdominal or flank pain, hypotension, and a pulsatile mass occur in only half of patients presenting with a ruptured AAA (rAAA) [6]. Symptoms may be vague complaints of back, abdominal, or flank pain, but can also mimic renal colic, diverticulitis, or gastrointestinal hemorrhage [1]. With such variation in presentation, timely diagnosis hinges on high clinical suspicion and a low threshold to ultrasound at the bedside in patients >50 y/o presenting with abdominal, flank or back pain.
Emergency Physicians Can Perform Accurate Bedside Ultrasound
In the emergency setting, bedside ultrasound has high clinical utility for narrowing the differential in a patient with vascular risk factors presenting with pain concerning for rAAA. A bedside ultrasound of the abdominal aorta is fast, noninvasive, inexpensive, and easy to perform. In a systematic review, Rubano et al. evaluated studies that included 655 patients with suspected AAAs and found that ED ultrasound for the detection of AAA had a sensitivity of 99% (95% CI = 96% to 100%) and specificity of 98% (95% CI = 97% to 99%) [7]
A bedside ultrasound of the entire length of the abdominal aorta can be completed in 2-3 minutes. For stepwise instruction on bedside abdominal aortic ultrasounds see:
EM Curious
Sonoguide (site currently under construction)
An Algorithmic Approach to Imaging in Symptomatic AAA
In stable patients with suspected symptomatic AAAs, imaging strategy depends on the clinical status of the patient (see above algorithm). While CT is considered the gold standard for diagnosis and provides useful information regarding surgical planning (endovascular versus open repair), in a hemodynamically unstable patient, obtaining this study is not possible and we must rely on bedside ultrasound to make the diagnosis. In patients with a known AAA, abdominal pain, and hypotension, rAAA should be presumed and vascular surgery should be consulted immediately for operative repair.
Case Resolution
CT illustrated a 7.5 cm infrarenal AAA that was rupturing into the retroperitoneal space. He was taken to the OR for endovascular repair and discharged home six days later.
"Aneurysm of the abdominal aorta is very often diagnosed when not present, and when present the symptoms may be so obscure that the nature of the trouble is overlooked." -William Osler
Take Home Points:
- It is easy to miss a symptomatic AAA, and failing to consider it in the differential can be catastrophic
- Beside US for suspected AAA by emergency physicians can be performed efficiently and accurately
- Consider a quick bedside abdominal aorta ultrasound scan as part of your physical exam in any older patient with vascular risk factors complaining of back, flank, or abdominal pain
- Imaging for suspected symptomatic AAA should be based on the patient's clinical status and you should have a low threshold to have vascular surgery on board early
Expert Commentary
Thank you Dr. Ford for this succinct review of this classic emergency. Since this algorithmic approach is so simple, I’ll add just some details to round it out:
Who needs AAA ruled out:
Anyone with a physiologic or chronologic age over 50 with:
Abdomino-pelvic pain
Dizziness NOS
Hypotension NOS
Syncope
Atraumatic lumbar radiculopathy
If you can’t get an adequate ultrasound:
This isn’t the time to get stingy on radiation or contrast. Get at least a non-contrast CT of the belly and go with them to the scanner. Consider whether or not your vascular surgeons prefer a CTA; if you see a AAA on the non-contrast scan, you can get a CTA without delay. These patients are sick, so the urgency of diagnosis likely trumps the marginal risk of contrast-induced nephropathy. Most don’t wait for a creatinine result for CTAs in strokes, so why wait for this? If you’re worried about giving contrast, no big deal; you can still get most essential information from a plain scan.
Non-ruptured AAA on CT:
Call vascular surgery regardless of symptoms. If the patient has symptoms that can be ascribed to the AAA, you’ll admit for observation (consider the ICU) and possible repair. If the patient’s symptoms can be explained with certainty by something else and the aneurysm is relatively small (<6 cm), you can likely arrange outpatient follow-up with the surgeon. Ensure these patients quit smoking and start exercising.
When to transfer out from a non-vascular medical center:
As soon as safely possible after you have an US or CT with AAA and compatible symptoms.
Lucas Rosiere, MD
Health System Clinician of Emergency Medicine
Feinberg School of Medicine, Northwestern University
Other Posts You May Enjoy
How to cite this post
[Peer-Reviewed, Web Publication] Ford W, Marshall A (2017, Aug 1). AAA-Ok: Approach to Imaging of Abdominal Aortic Aneurysm. [NUEM Blog. Expert Commentary By Rosiere L]. Retrieved from http://www.nuemblog.com/blog/aaa-ultrasound
References
- Adams, James. Emergency Medicine: Clinical Essentials. Philadelphia, PA: Elsevier/Saunders, 2013. Print.
- Bush, RL, PH Lin, and AB Lumsden. Endovascular Management of Abdominal Aortic Aneurysms. J Cardiovasc Surg 44.4 (2003): Aug. 2003. Web.
- Cadogan, M. Ultrasound in Emergency Medicine and Critical Care. LITFL Life in the Fast Lane Medical Blog. Attribution-NonCommercial-ShareAlike 4.0 International, 03 Oct. 2012. Web.20 Nov. 2015. http://lifeinthefastlane.com/ultrasound-in- emergency-medicine/
- Dean, A., and B. Ku. “Abdominal Aortic Aneurysm” Ultrasound Guide for Emergency Physicians, 2008. Web. 21 Nov. 2015. http://www.sonoguide.com/abdominal_aortic_aneurysm
- Marston, WA, et al. “Misdiagnosis of ruptured abdominal aortic aneurysms.” J Vasc Surg 1992; 16:17. Web.
- Rickenbach S, et al. “Prehospital treatment of intrarenal ruptured abdominal aortic aneurysms: a multicentric analysis.” Ann Vasc Surg 2010; 24:308.Web.
- Rubano, Elizabeth, Ninfa Mehta, William Caputo, Lorenzo Paladino, and Richard Sinert.Systematic Review: Emergency Department Bedside Ultrasonography for Diagnosing Suspected Abdominal Aortic Aneurysm. Acad Emerg Med Academic Emergency Medicine 20.2 (2013): 128-38. Web.
- Tayal VS, et al: Prospective study of accuracy and outcome of emergency ultrasound for abdominal aortic aneurysm over 2 years. Acad Emerg Med10:867-871 2003. Web.
- Tintinalli, Judith E., and J. Stephan. Stapczynski. Tintinalli's Emergency Medicine: A Comprehensive Study Guide. 7th ed. New York: McGraw-Hill, 2011. Print.