What should you do for patients who fall victim to riot control agents?
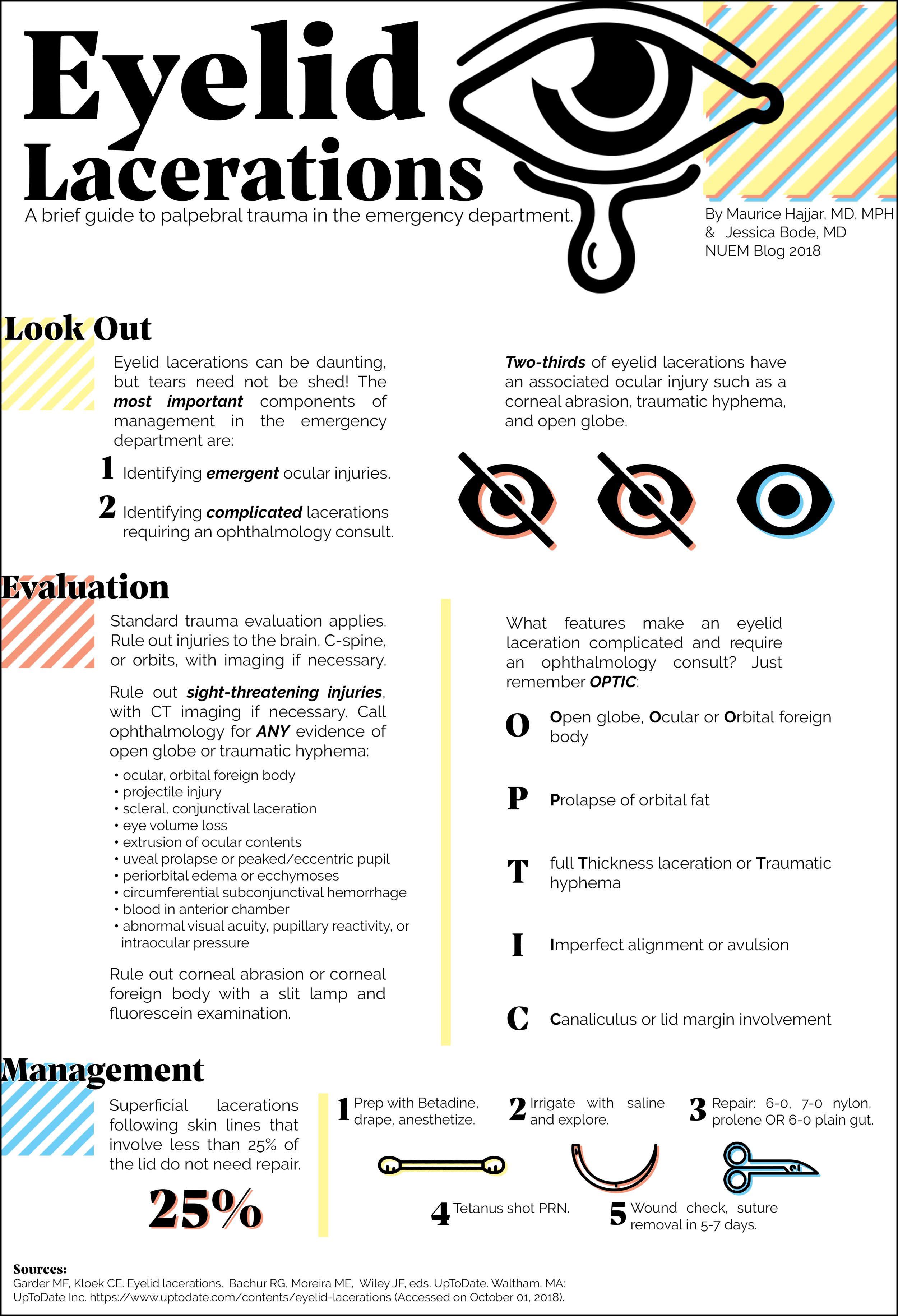
Eyelid Lacerations
Written by: Maurice Hajjar, MD (PGY-2) Edited by: Jessica Bode, MD (NUEM ‘19) Expert Commentary by: Rehan Hussain
Expert Commentary
Thank you for this excellent diagram, which demonstrates a thorough and systematic approach to eyelid lacerations encountered in the Emergency Room. I have a few extra pearls that may aid ER physicians in management of eyelid lacerations.
Be suspicious in glancing blunt trauma to the cheek or zygoma. This type of blow puts a great deal of stress on the medial canthal anatomy and may result in avulsion of the medial canthus with coexistent canaliculus laceration. This type of laceration may be missed because of the blunt mechanism and because the medial canthal tissues often reappose into a reasonable position, masking the extent of the injury. Look for displacement, excessive rounding, or abnormal laxity of the medial canthus.
Dog bites are notorious for causing canalicular lacerations. Canalicular probing should be performed in all such cases, even with lacerations that appear to be superficial. In some cases, debridement of necrotic tissue is warranted. With uncooperative children, conscious sedation or examination under anesthesia is often necessary to thoroughly examine the eyelids and globes. Administer systemic antibiotics if contamination or foreign body is suspected. For animal bites, consider rabies prophylaxis if warranted. Note that canalicular lacerations are not an ophthalmological emergency and repair can be delayed for 3-7 days without long term negative effects.
Visible orbital fat in an eyelid laceration indicates penetration of the orbital septum, and all such patients require CT imaging and documentation of levator and extraocular muscle function. Exploration of deeper tissue planes may be needed and ophthalmology consultation is warranted. Do not remove any foreign body prior to surgery if there is a possibility of globe penetration or extension into the orbit – this is best performed in a controlled OR environment. A multi-disciplinary approach may be necessary with ophthalmology and possibly ENT or neurosurgery depending on the extent of the injury.
When repairing lacerations, try to not overdo the subcutaneous lidocaine, because it can cause tissue distortion and make the repair more challenging, though you must find a balance to keep the patient comfortable during the repair. It is advisable to place a drop of proparacaine and a protective shell over the eye to prevent any inadvertent globe trauma. I prefer to use absorbable vicryl or gut sutures in children or if the patient seems unlikely to follow up. I enjoy your clever OPTIC mnemonic, and agree all of those listed scenarios should result in an ophthalmology consult.
Rehan M. Hussain, MD
Ophthalmology
Retina Associates, Ltd
How to Cite this Post
[Peer-Reviewed, Web Publication] Hajjar, M, Bode, J. (2020, May 4). Eyelid Lacerations [NUEM Blog. Expert Commentary by Hussain, R]. Retrieved from http://www.nuemblog.com/blog/eyelid-lac
Approach to Double Vision in the ED
Written by: Andy Rogers, MD (NUEM PGY-2) Edited by: Dana Loke, MD (NUEM PGY-4) Expert commentary by: Quentin Reuter, MD
Seeing double: toil and trouble?
Introduction
Double vision, or diplopia, is a relatively infrequent presenting symptom in the emergency setting, representing 0.1% of Emergency Department (ED) complaints (1). Diplopia can result from benign processes, such as dry eyes or idiopathic cranial nerve palsy, to emergent conditions with high morbidity, such as stroke, aneurysm, or inflammatory processes. Given a wide range of possible outcomes for a less common presenting complaint, it is worth reviewing the neuroanatomy and etiologies of diplopia, as well as a generalized approach to the patient presenting to the ED with double vision.
Neuroanatomy
The neuroanatomy underlying control of the extraocular muscles and their ability to provide gaze alignment is complex and worth a brief review. Eye movements are governed by six extraocular muscles, which are controlled by four cranial nerves, summarized in Table 1 and Figure 1 below. The nuclei for the cranial nerves are located in the brainstem. The nerves course from the brainstem, through the subarachnoid space, the cavernous sinus (Figure 2), the orbital apex, and finally to their respective extraocular muscles. Given the close proximity of nearby structures, lesions can often be localized based on associated symptoms, in addition to gaze palsies, to help guide workup and diagnosis. For instance, an important additional function of CN III includes the parasympathetic fibers that travel along the oculomotor nerve that contribute to pupillary constriction.
Table 1: Summary of functions of the extraocular muscles, grouped by cranial nerve. (2)
Figure 1: Diagnostic positions of gaze with associated extraocular muscles contributing to movement. (3)
Figure 2: Cavernous sinus and its contents. Note that the cavernous sinus is symmetric about the pituitary fossa (only one side is shown above) (4)
Initial approach to diplopia
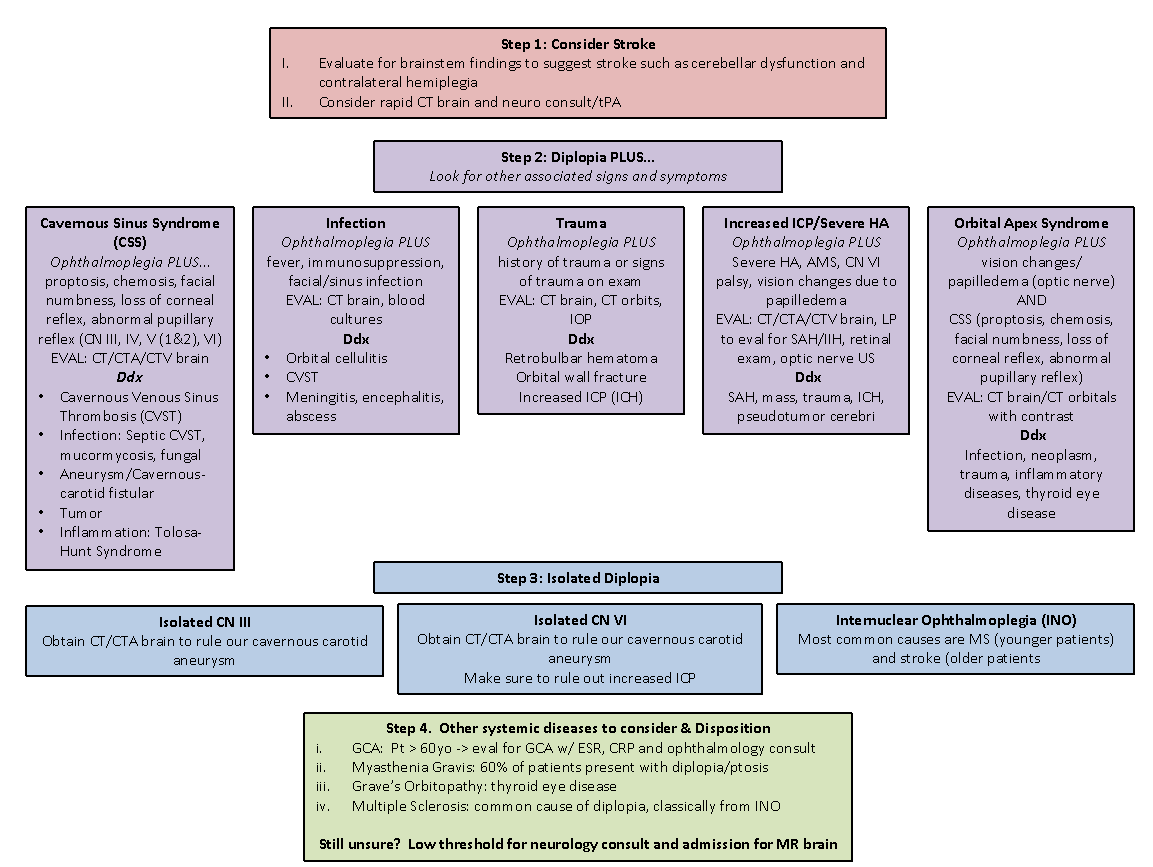
Dr. Margolin and Dr. Lam published an excellent review of the approach to diplopia in the ED, summarized in Figure 3 (5). Critical to the diagnosis is a good history and neurologic exam. Their approach involves the follow steps:
Determine if symptoms are monocular or binocular
Determine if there are associated neurologic signs or symptoms
If isolated diplopia, determine if the palsy localizes to a third or sixth nerve palsy, or if it is a complex motility disorder
Screen for giant cell arteritis (also known as temporal arteritis) in all patients over the age of 60
Figure 3: Approach to patient with diplopia, from Margolin and Lam (5)
Monocular or Binocular
The first step in the approach to diplopia in the ED is to determine if the diplopia is monocular or binocular. Some patients may not know or not have checked prior to presentation. Ask the patient “does the double vision resolve when you close one eye?”
Monocular Diplopia
Monocular diplopia persists with one eye closed. This localizes the lesions to the affected eye and reflects that the issue is not with misalignment of gaze. It is almost always benign and most often due to dry eyes and refractive error (5, 6). Referral to an ophthalmologist is appropriate and no further imaging is indicated unless warranted by other features of the patient’s presentation.
Binocular diplopia
Binocular diplopia resolves with one eye closed. This indicates ocular misalignment that can be due to an issue with the muscle, nerve, or CNS.
Binocular diplopia with associated neurologic signs
Diplopia with other associated neurologic signs is concerning. Acute onset of symptoms may be due to intracranial hemorrhage, cerebrovascular disease, or rapidly progressive neurologic disorder. Initiation of stroke protocol is valuable for several reasons. It allows for rapid diagnosis of hemorrhagic or ischemic stroke, evaluates for cerebral aneurysm, and involves Neurology quickly in the patient’s care. Some neurologic signs and symptoms, or clusters of signs and symptoms can help identify the etiology (5-7). See Table 2 below.
Binocular diplopia without associated neurologic signs (Isolated diplopia)
In all patients presenting with diplopia, careful examination of the extraocular movements and pupils are important to localizing the lesion. Note that diplopia can be due to weakness in one direction or entrapment of the muscle limiting range of motion. Both etiologies must be kept in mind. Figure 1 is a good reference to identify what muscles and nerves may be affected based on directional limitations in extraocular movements. Some important questions to ask include (6):
Are the two images side by side, on top of each other, or on a diagonal? – helps to tease out the plane of action of the affected muscles and their respective nerves
What field of gaze makes the double vision worse? – this represents the field of vision of a paretic muscle or opposite the field of action of a restricted muscle
Can you move your head to correct the vision? – Oblique diplopia due to CN IV paresis often can be distinguished with tilting of the head. Vertical diplopia can be improved with neck extension or flexion.
Is there pain with eye movement? – suggests myopathy or orbital process
Isolated 4th nerve palsies:
The trochlear nerve innervates the superior oblique muscle. Patients often complain of vertical or diagonal diplopia that may correct with head tilt. CN IV palsies are most commonly due to trauma or are idiopathic in nature (6). In idiopathic CN IV palsies, the patient should be referred to ophthalmology. The palsy often resolves within two weeks. Important neurologic signs to look for with a CN IV palsy are cerebellar signs. The trochlear nerve exits on the dorsum of the brainstem and may be compressed by a posterior fossa tumor.
Isolated 6th nerve palsies:
The abducens nerve, or 6th cranial nerve, innervates the lateral rectus muscle. In a 6th nerve plasy, patients will complain of a horizontal diplopia. There is often inward deviation of the affected eye (esotropia) and symptoms are made worse with lateral gaze to the affected side (6). This nerve palsy is often idiopathic in etiology, with diabetes mellitus as a risk factor. Be careful to assess for bilateral 6th nerve palsy. The abducens nerve has a long, isolated course intracranially; tumors can affect the bilateral abducens nerve before other areas of the brain are affected.
Isolated 3rd nerve palsy:
The oculomotor nerve innervates four muscles and carries parasympathetic fibers that control pupil constriction. Its course is closely related to the posterior cerebral artery and posterior communicating artery. A palsy of the 3rd nerve (especially with pupillary involvement) may be due to cerebral aneurysm and must emergently be evaluated with CTA, MRA, or intravascular angiography. An acute isolated 3rd nerve palsy may be due to expanding aneurysm that is at risk of imminent rupture (7). Pupil sparing 3rd nerve is rarely due to an aneurysm and more often ischemic injury (6,7).
Internuclear ophthalmoplegia (INO)
In the setting of horizonal diplopia, also look for internuclear ophthalmoplegia (INO). An INO is impaired horizontal movement with weak adduction of the affected eye and abduction nystagmus of contralateral eye (8). This localizes the lesion to the medial longitudinal fasciculous (MLF) in the dorsomedial brainstem tegmentum. The MLF connects the 6th nerve nucleus and medial rectus subnucleus of the 3rd nerve nucleus to coordinate lateral conjugate gaze movement. In patients <45 years old, it is most commonly caused by multiple sclerosis and is often bilateral (73%) (9). In older patients, especially those with vascular risk factors, it is caused by cerebrovascular disease and is usually unilateral. Up to a third have other causes, including infection, tumor, trauma, myasthenia gravis, and Guillain-Barre. Look for historical clues and other neurologic exam findings. Presence of an INO requires MRI workup.
Complex motility abnormality
If the diplopia doesn’t isolate to a specific cranial nerve, consider what nerves may be involved and where they are close together to consider anatomic abnormalities. This includes the cavernous sinus, orbital apex, and brainstem. Brainstem lesions will often have other neurologic deficits identified on exam.
Cavernous sinus
Cavernous sinus lesions will affect multiple cranial nerves but should not affect visual acuity as the optic nerve does not pass through in relation to the other structures (5,7). The pituitary gland also resides between the cavernous sinuses. Pituitary mass or apoplexy can compress laterally causing ophthalmoplegia. Another key concern is septic cavernous sinus thrombosis. These patients will often be septic and febrile. Conversely, consider asking your septic patients if they have double vision! Consider CT and CT venogram of brain and orbits.
Orbital apex
The orbital apex involves all extraocular muscles, sympathetic fibers, and cranial nerves 2/3/4/6/V1/V2. Here, the optic nerve is in close anatomic relation to the nerves and muscles of ocular motility. Any ophthalmoplegia with decreased vision or numbness in V1 or V2 distribution should raise concern for orbital apex pathology (5,7). Consider CT with contrast of the orbits.
Giant Cell Arteritis
Giant cell arteritis (also known as temporal arteritis) is an important diagnosis to always consider in an elderly patient presenting with diplopia. Missing this diagnosis can lead to permanent vision loss. Diplopia is actually an uncommon finding in GCA, occurring in roughly 5% of cases. However, diplopia has the second highest positive likelihood ratio (LR 3.4) for GCA (the highest being jaw claudication – LR 4.2) (10). In an elderly patient presenting with diplopia, be on the lookout for other signs and symptoms suggestive of GCA, such as jaw claudication, fevers, vision loss, temporal headaches, PMR, or elevated inflammatory markers.
Key Points
Diplopia is a relatively rare presenting complaint in the Emergency Department, and it can portend a wide range of disease, from the benign to the emergent
A good history and physical exam are key to diagnosis
Use your physical exam and the presence of other neurologic signs and symptoms to try to localize the lesion and guide imaging choice
Screen for temporal arteritis in the >60 population
Expert Commentary
Diplopia is a rare but potentially dangerous chief complaint, making up approximately 0.1% of all ED visits. [1] In one study of 260 ED patients with non-traumatic, binocular diplopia, 64% had primary diplopia (i.e. no identifiable cause found, likely from microvascular ischemic disease) and 36% had secondary diplopia (i.e. caused by some discernible pathology). Of patients with secondary diplopia, stroke accounted for nearly 50%, with multiple sclerosis (MS), tumor, aneurysm, myasthenia gravis (MG), and carotid cavernous fistula (CCF) accounting for the other diagnoses. [1] Given the dangerous etiologies at play, clinicians must approach these patients in a systematic and cautious manner. (Figure 1)
In patients presenting with diplopia, the first concern must be the possibility of stroke and the need to consider time-sensitive treatment with thrombolytics. Cranial nerves (CN) 3, 4, and 6 are supplied by the vertebrobasilar arterial system and strokes affecting these nerves most often present with cerebellar dysfunction and/or “crossed signs” or contralateral hemiparesis from involvement of the corticospinal tracts. [2] Thrombolytic treatment must be considered if the patient is presenting within the appropriate time window and stroke is suspected. If the patient is outside of the tPA window but suspicion remains for an ischemic process, these patients may benefit from neurologic consultation and MR imaging.
After considering stroke, look for other associated signs or symptoms that may lead to the correct diagnosis. If a patient has fevers, facial infections, or meningismus one must consider orbital cellulitis, cavernous venous sinus thrombosis (CVST), meningitis, or encephalitis. If a patient had a traumatic injury, consider orbital wall fractures, retrobulbar hematoma, increased intracranial pressure (ICP), and intracranial hemorrhage. If a patient has proptosis, chemosis, headaches, and/or facial sensory changes, consider cavernous sinus pathology such as CCF, aneurysm, CVST, mass, or Tolosa-Hunt syndrome (idiopathic inflammatory changes within the cavernous sinus). If a patient has a severe headache, CN 6 palsy, and/or AMS, consider subarachnoid hemorrhage or other causes of increased ICP. Notably, up to 5% of ruptured PCOM aneurysms present with a CN 6 palsy. [3] Lastly, if patients have concomitant vision changes/loss, consider pathology of the orbital apex such as mass, infection, and thyroid eye disease.
If no associated signs or symptoms exists, evaluate the patient for an isolated CN palsy. (Figure 2) The Margolin paper discusses the importance of obtaining a CTA brain in patients with isolated CN 3 palsy to rule out an intracranial aneurysm. I would also highlight the importance of obtaining a CTA when patients have an isolated CN 6 palsy as 16% of patients with cavernous sinus carotid aneurysm presented with isolated CN 6 palsy in one study. [4] In patients with internuclear ophthalmoplegia (INO), admission for MR and neurology consultation is appropriate to rule out stroke and MS, the most common causative pathologies. Finally, clinicians must consider systemic disease entities such as giant cell arteritis (GCA), MS, and MG. GCA is a vision-threatening disease and must be considered in patients over the age of 60 with transient or persistent diplopia as it is a presenting complaint in 6-27% GCA patients. [5]
Finally, a word of caution when approaching patients with diplopia. The Margolin article suggests that some patients with isolated diplopia can have non-emergent outpatient follow-up once an aneurysm has been excluded. Others have also recommended that a CT brain is not useful in the setting of isolated diplopia citing one study showing CT had a sensitivity of 0% in 11 patients with isolated secondary diplopia as the rationale. [6] I believe these recommendations are unrealistic for many reasons. First, diplopia is encountered only infrequently in the ED, making the gains of avoiding a CT brain and inpatient neurologic workup minimal. Furthermore, the neuro-ophthalmologic exam is challenging, and some patients can present with partial palsies or deficits involving multiple cranial nerves, making diagnosis of a specific CN challenging. Clinicians must also be 100% confident that no other signs or symptoms exist such as jaw claudication in GCA or subtle vision changes and papilledema for pseudotumor cerebri prior to discharge, a difficult task in a busy ED. Ensuring reliable and urgent neurologic follow-up and outpatient MR imaging can also be difficult or impossible in many health systems. Patients will also likely appreciate obtaining a definitive diagnosis for a concerning neurologic symptom like diplopia in a timely manner. Moreover, of the 11 patients with isolated secondary diplopia for which CT was not useful in the Nazerian article, two had strokes, another patient had a mass, and another had a CFF that the CT missed. [1] Diagnoses such as stroke, aneurysm, MS, GCA, and neoplasm can all have morbid ramifications if not expediently diagnosed.
As such, in patients with isolated diplopia, it may be appropriate for ED clinicians to rule out aneurysm with vascular imaging and admit for neurology consultation and MR to evaluate for more sinister pathology. ED clinicians should at the very least discuss the case with a consulting neurologist to ensure appropriate management. While the majority of patients with isolated diplopia will go on to be diagnosed with microangiopathic ischemia, given the above concerns, it would seem reasonable for ED clinicians to err on the side of caution and get help from their local neurology colleagues for these challenging patients.
Citations:
1. Nazerian P, Vanni S, Tarocchi C, et al. Causes of diplopia in the emergency department: diagnostic accuracy of clinical assessment and of head computed tomography. Eur J Emerg Med 2014;21:118-24.
2. Rowe F, UK VISg. Prevalence of ocular motor cranial nerve palsy and associations following stroke. Eye (Lond) 2011;25:881-7.
3. Burkhardt JK, Winkler EA, Lasker GF, Yue JK, Lawton MT. Isolated abducens nerve palsy associated with subarachnoid hemorrhage: a localizing sign of ruptured posterior inferior cerebellar artery aneurysms. J Neurosurg 2018;128:1830-8.
4. Stiebel-Kalish H, Kalish Y, Bar-On RH, et al. Presentation, natural history, and management of carotid cavernous aneurysms. Neurosurgery 2005;57:850-7; discussion -7.
5. Haering M, Holbro A, Todorova MG, et al. Incidence and prognostic implications of diplopia in patients with giant cell arteritis. J Rheumatol 2014;41:1562-4.
6.Kisilevsky E, Kaplan A, Micieli J, McGowan M, Mackinnon D, Margolin E. Computed tomography only useful for selected patients presenting with primary eye complaints in the emergency department. Am J Emerg Med 2018;36:162-4.
Figure 1: Approach to the patient with diplopia
Figure 2: Clinical exam for CN 3 palsy, CN 6 palsy, and INO
Figure 2A: Complete CN 3 palsy
Figure 2B: Complete CN 6 palsy
Figure 2C: Internuclear Ophthalmoplegia
Quentin Reuter, MD
Assistant Professor of Emergency Medicine
Northeast Ohio Medical University
Citations
Sources:
“Causes of Diplopia in the Emergency Department: Diagnostic Accuracy of Clinical Assessment and of Head Computed Tomography.” Nazerian et al. European Journal of Emergency Medicine. 21 April 2014 (2):118-24. Doi 10.097/MEJ.0b01323283636120
“Actions of Extraocular Muscles.” UpToDate.com. Accessed 11/22/18.
Image adapted from: “Diagnostic Positions of Gaze.” UpToDate.com Accessed 11/22/18.
Image from: “ZSFG Neuro Report: Multiple Cranial Neuropathies – Spotlight on the Cavernous Sinus.” Stern, Rachel. UCSF Internal Medicine Chief Resident Hub. Published 28 Oct 2016. Accessed 20 November 2018. https://ucsfmed.wordpress.com/2016/10/28/zsfg-neuro-report-multiple-cranial-neuropathies-spotlight-on-the-cavernous-sinus/
“Approach to a Patient with Diplopia in the Emergency Department.” Margolin, Edward and Lam, Cindy. Journal of Emergency Medicine. Volume 54, Issue 6. June 2018. pp799-806. Accessed 16 November 2018.
“Overview of Diplopia.” Bienfang, Don. UpToDate. Last updated 20 June 2017. Accessed 17 November 2018.
“Third Cranial Nerve (Oculomotor Nerve) Palsy in Adults.” Lee, Andrew. UpToDate. Last updated 19 June 2017. Accessed 17 November 2018.
“Internuclear Ophthalmoparesis.” Frohman, Teresa; Frohman, Elliot. UpToDate. Last updated 4 December 2017. Accessed 18 November 2018.
“Internuclear Ophthalmoplegia Unusual Causes in 114 of 410 Patients.” Keane, James. Arch Neurol. 2005;62(5):714–717. doi:10.1001/archneur.62.5.714
“Does This Patient Have Temporal Arteritis?” Smetana, Gerald; Shmerling, Robert. JAMA. 2002;287(1):92–101. doi:10.1001/jama.287.1.92
How To Cite This Post
[Peer-Reviewed, Web Publication] Rogers A, Loke D. (2019, Nov 18). Approach to Double Vision in the ED. [NUEM Blog. Expert Commentary by Reuter Q]. Retrieved from http://www.nuemblog.com/blog/double-vision.
Other Posts You May Enjoy
Tetracaine
Written by: Jonathan Hung, MD, (NUEM PGY-3) Edited by: Matt Klein, MD (NUEM ‘18) Expert commentary by: Dr. Glaucomflecken
Introduction
Corneal abrasions are a commonly encountered eye-related presentation in the emergency department (ED) [1]. Patients will often have a significant amount of pain from even minor abrasions. Topical anesthetics such as tetracaine have been found to be effective in treating the pain and are now routinely used in the ED [2]. However, the use of topical anesthetics for corneal abrasions in the outpatient setting is controversial due to concerns over safety and delayed healing. These traditional concerns over the prolonged use of topical anesthetics are based on early animal studies and case reports in humans [3]. The current literature suggests that topical anesthetics are, in fact, safe and effective if given as a short course with appropriate follow up, but further studies with larger patient populations are needed to support these findings [4]. A recent study published in Annals of Emergency Medicine is one of the largest studies to date that examines the safety of discharging patients home from the ED with a short supply of tetracaine for corneal abrasions.
Study
Waldman N, Winrow B, Densie I, et al. An Observational Study to Determine Whether Routinely Sending Patients Home With a 24-Hour Supply of Topical Tetracaine From the Emergency Department for Simple Corneal Abrasion Pain Is Potentially Safe. Ann Emerg Med. 2017.
Study Design
The study design was a single-center, retrospective cohort study with ethics approval given by the Human Ethics Committee at the University of Otago.
Population
The study was performed at the ED of Southland Hospital, Invercargill, New Zealand. A computer search of the hospital’s ED information system was conducted looking for all eye-related diagnoses and charts were reviewed between February 1, 2014 to October 31, 2015. Patients were initially selected if they were seen in the ED with an injury or illness involving the cornea.
Intervention protocol
Patients with simple corneal abrasions were discharged home with undiluted 1% tetracaine hydrochloride in addition to the standard treatment of acetaminophen and chloramphenicol eye ointment. Instructions were given to place tetracaine in the eye as often as every 30 minute over the first 24 hours.
Outcome Measures
ED rechecks
Persistent fluorescein uptake
Ophthalmology clinic referrals
Complications
Results
There was a total of 1,576 ED presentations of corneal abrasions of which 532 were simple corneal abrasions (SCA) and 1,044 were defined as nonsimple corneal abrasions (NSCA). Tetracaine was given to 57% (303) of SCA patients and 14% (141) of NSCA patients. Overall, there were no serious complications or uncommon adverse events in either the SCA or NSCA group (0/459). The relative risk of patients with SCA receiving tetracaine and returning to the ED, having fluorescein uptake, or requiring a referral to ophthalmology was low compared to the standard treatment group.
Interpretation
This study is one of the largest studies to examine the safety of outpatient tetracaine use in simple corneal abrasions. More importantly, it gives a robust conclusion similar to previous smaller studies in that there was no evidence that using topical tetracaine for a short duration caused harm. The strengths of this study include the large patient population and good patient follow-up. Furthermore, the physicians that administered tetracaine did not know that an observational study was planned, thus increasing the internal validity. However, the researchers were not blinded to the hypothesis which could have led to bias when collecting data. This was also a retrospective study and therefore due to the lack of randomization, those who received tetracaine may have differed from those who did not. Another limitation was that it was not known if all the patients administered the tetracaine as instructed after leaving the ED. Also, the diagnosis of simple corneal abrasion was limited to what the physician documented in the chart. The external validity is limited since this was a single-center study and about 71% of the patients were males. Overall, this study further strengthens the role of tetracaine in treating pain secondary to simple corneal abrasions and may gradually change practice patterns in the emergency department despite traditional teaching.
Take Home Points
Topical tetracaine is effective in treating pain due to corneal abrasions
Patients with simple corneal abrasions can benefit from a short course of topical tetracaine to treat pain
Topical tetracaine use over a 24-hour period is generally safe
Emergency medicine physicians should consider incorporating topical tetracaine in their practice for treating SCAs
Expert Commentary
This is an interesting observational study regarding the safety of prescribing a limited supply of topical tetracaine to patients who present to the emergency department with what the authors describe as “simple corneal abrasions.” It is well documented in the literature that long term use of topical anesthetics can lead to a variety of serious ophthalmic complications, including persistent epithelial defects, neurotrophic ulceration, secondary infectious keratitis, corneal scarring and perforation. However, many of these reports describe long term use of anesthetics ranging from 7 days to 6 months which have helped establish the long-held dogma that topical anesthetics are only appropriate for use during surgery or clinic examination. This study, as well as several smaller previous studies, has attempted to challenge that dogma in an effort to better treat the immense pain often associated with corneal abrasion.
The authors did a great job trying to distinguish between simple and non-simple corneal abrasions. This can be very difficult, even for an ophthalmologist. What may look like a simple corneal abrasion can easily turn out to be a different diagnosis altogether. Herpes simplex keratitis can present as a geographic ulcer, lighting up with fluorescein much like a corneal abrasion without the tell-tale sign of dendritic lesions to accompany it. Dry eye disease can result in confluent, punctate epithelial defects which can look like a corneal abrasion without the magnification afforded by a slit lamp. These conditions should not be treated with topical anesthetics and will only delay the patient in receiving appropriate care. Stating that topical anesthetics are safe for simple corneal abrasions assumes that the examiner is able to accurately diagnose a simple abrasion. In this study, several patients were misdiagnosed as simple abrasions and ultimately required follow up with ophthalmology. Patients who need to see ophthalmology for a non-simple abrasion may be less likely to follow up in a timely manner if they are given topical anesthetic that will effectively mask the pain. This can result in more extensive corneal scarring from a variety of diagnoses such as delayed rust ring removal or treatment of infectious keratitis.
The authors make a compelling point that a limited supply of tetracaine in a subset of corneal abrasions intended to last no more than 24 hours is safe with no significant difference in the number of ED rechecks, ophthalmology clinic referrals, persistent fluorescein uptake, or complications. If this is indeed true, is treating with topical anesthetic worth it? At best, you are providing a minimally-painful healing process which will be complete in 48-72 hours regardless of topical anesthetic use. At worst, you are masking pain of a potentially vision-threatening process that may have been misdiagnosed as a simple abrasion. I contend that setting patient expectations regarding pain (very severe for first 24 hours, then rapid improvement) and discussing more conservative comfort measures like icing and patching are sufficient.
Lastly, I want to discuss the treatment for simple and non-simple corneal abrasions. It is unclear whether or not the patients in this study were treated with topical antibiotics. It is possible that patients with simple corneal abrasions were sent home with a 24 hour supply of tetracaine and no topical antibiotics. Without an epithelial barrier, the underlying corneal stromal is prone to infection. Topical antibiotics act as a preventive measure and are particularly important if a patient is using topical anesthetic, which could mask the pain of infectious keratitis. Although not all sources agree, there is general consensus among ophthalmologists that all corneal abrasions require topical antibiotics at the time of diagnosis.
In conclusion, I agree that a 24 hour prescription of topical anesthetic in a simple corneal abrasion is likely safe. However, given the rapid healing time, consideration should be made to counseling patients on pain expectation and comfort measures in place of topical anesthetic. Lastly, prescribing more than a 1 day supply of topical anesthetic is unnecessary given the rapid improvement in pain after the first 24 hours
Dr. Glaucomflecken, MD
https://www.drgcomedy.com/
https://twitter.com/dglaucomflecken
http://gomerblog.com/author/glaucomflecken/
How To Cite This Post
[Peer-Reviewed, Web Publication] Hung J, Klein M. (2019, July 8). Tetracaine. [NUEM Blog. Expert Commentary by Dr. Glaucomflecken]. Retrieved from http://www.nuemblog.com/blog/tetracaine.
Other Posts You May Enjoy
References
Verma A, Khan FH. Corneal abrasion. MedscapeAvailable at: http://emedicine.medscape.com/article/1195402-overview. Accessed November 1, 2017.
Waldman N, Densie IK, Herbison P. Topical tetracaine used for 24 hours is safe and rated highly effective by patients for the treatment of pain caused by corneal abrasions: a double-blind, randomized clinical trial. Acad Emerg Med 2014;21:374–82.
Chang YS, Tseng SY, Tseng SH, et al. Cytotoxicity of lidocaine or bupivacaine on corneal endothelial cells in a rabbit model. Cornea 2006;25:590–6.
Swaminathan A, Otterness K, Milne K, Rezaie S. The Safety of Topical Anesthetics in the Treatment of Corneal Abrasions: A Review. J Emerg Med. 2015;49(5):810-815.
Corneal Abrasions
Written by: Julian Richardson, MD, MBA (NUEM PGY-2) Edited by: Andrew Moore, MD (NUEM ‘18) Expert commentary by: Brad Sobolewski, MD, MEd
A 40 yo construction worker comes to Emergency Department with a foreign body sensation in his left eye for two days. He states that he forgot to wear his eye protection while sanding a plank of wood the other day and felt like something has been scratching his eye ever since. Upon entering the room, his left eye is hyperemic and the patient appears to be in discomfort.
Approach to the painful red eye with foreign body sensation
The initial differential diagnosis to a painful red eye is broad and includes entities such as keratitis, corneal abrasions, corneal ulceration, acute angle glaucoma, iritis, chemical burn, scleritis, subconjunctival hemorrhage, and conjunctivitis. The patient’s history is particularly concerning for corneal abrasion, corneal ulceration, or globe rupture. A simple test to distinguish these diagnoses is the fluorescein exam.
Fluorescein exam
Fluorescein has been used in ophthalmology since the 1880s. This exam should be included for all patients where there is a suspicion of abrasion, foreign body, or infection. Fluorescein absorbs light in blue-wavelengths and emits energy in green wavelengths. It fluoresces in alkaline environments, for example Bowman’s membrane which is located below the corneal epithelium. It does not fluoresce in acidic environments such as the tear film over intact cornea. Because of this, defects in the cornea increase fluorescein uptake and assist in locating corneal damage.
The eye should first be numbed usually with the use of a topical anesthetic drop, such as tetracaine. Next, take a fluorescein strip and place one drop of saline or local anesthetic to the strip. Place this strip inside the lower lid, remove, and ask the patient to blink. The key to a good exam is to produce a thin layer covering the surface of the eye. If too much is applied, the excess can easily be removed by asking the patient to blot their eye while closed with a tissue. The eye should then be examined using a Wood’s lamp, blue filter of a slit lamp, or penlight with a blue filter
Warning! this dye will permanently stain soft contact lenses and clothing. Be sure to remove any contacts and have plenty of gauze or other absorbant material available prior to instillation. Irrigating the excess dye out the eye after examination will help minimize staining the patient’s clothing.
Corneal Abrasion
Definition
Scratch to the epithelium that comprises the cornea and exposes the basement membrane. Patients generally complain of a foreign body sensation, pain, photophobia, and some vision loss. On physical exam, the clinician may find injected conjunctiva, and decreased visual acuity (if the defect is large or lies in the visual axis).
Fluorescein Exam
Typically, abrasions are seen at the central part of the cornea due to limited protection of closure of the patient’s eyelids. The margins are sharp and linear in the first 24hrs. Circular defects suggests an embedded foreign body is present and may persist for greater than 48hrs. Foreign bodies can also produce vertical linear lesions and the upper lid should be lifter up to look for a foreign body under the eyelid
Management
Treatment with antibiotics have become the standard of care. Antibiotics are particularly indicated for abrasions caused by contacts (cover for pseudomonas), foreign bodies, or history of trauma with infectious or vegetative matter due to a higher risk of infection. Ophthalmic antibiotic therapy include: erythromycin ointment or sulfacetamide 10%, polymyxin/trimethoprim, ciprofloxacin, or ofloxacin drops (4 times a day for 3-5 days). Pain relief can be provided with oral or topical pain meds. Topical NSAIDs include .1% indomethacin, .03% flubiprofen, .5% ketorolac, 1% indomethacin, and .1% diclofenac. If symptoms persist greater than 24 hours after treatment the patient should follow-up with a physician. If the abrasion has not healed in 3-4 days the patient should be evaluated by an ophthalmologist.
Corneal Ulceration
Definition
When a defect in the corneal epithelium becomes infected with bacteria or fungi it is defined as a corneal ulceration. This is a common complication of corneal abrasions and if left untreated can result in a corneal perforation.
Fluorescein Exam
Corneal staining with infiltrate or opacification around the lesion should raise suspicion for ulceration. Contact lens wearers raise the suspicion of a Pseudomonal infection. Many Pseudomonal organisms fluoresce when exposed to UV light and fluoresce prior to fluorescein application.
Management
Concern for ulceration requires an urgent ophthalmology consultation within 24hrs. Discharged patients should be treated with antibiotic drops or ointment.
Globe Rupture
Definition
Full thickness injury to the cornea, sclera, or both secondary to penetrating of blunt trauma.
Fluorescein Exam
Seidel test: instill a large amount of fluorescein onto eye and looking for small stream of fluorescent blue or green fluid leaking from the globe.
Management
Once suspected, avoid further examination or manipulation, make the patient NPO, and place an emergent ophthalmology consultation. These patients also require broad spectrum IV antibiotic coverage with a 3rd generation cephalosporin or aminoglycoside and vancomycin to prevent post-traumatic endophthalmitis.
In summary, all patients with eye pain, particularly with a foreign body sensation, warrant a fluorescein exam. A wealth of information can be gained by this simple test and will guide the management of the patient.
Expert Commentary
This is a very comprehensive review of a common complaint in the Emergency Department. You correctly identified that one must be careful to avoid instilling too much fluorescein so as to cause a false positive result. Though a drop of tetracaine or saline dilutes the fluorescein from the strip somewhat the quantity is hard to control at times – especially in noncompliant patients (like the children I usually examine in the Pediatric Emergency Department). Excess fluorescein can collect across the eye making identification of small abrasions challenging. If you put too much in rinse the eye and try again. It is also incredibly important to not sent the patient home with tetracaine drops, as too frequent use may lead to further corneal injury. The evidence is based on animal models and case series and is far from complete. Read more on this great R.E.B.E.L. EM post (link: http://rebelem.com/topical-anesthetic-use-corneal-abrasions/).
One of the main pitfalls to the use of fluorescein strips is the risk of actually causing an abrasion. The method noted in this article – placing the strip inside the lower lid margin and asking the patient to blink – can cause an abrasion if the edge of the strip touches the cornea. This is particularly challenging to do in children, since even with proper restraint the blink reflex and their tendency to recoil is high. Therefore I recommend doing one of the following:
Hold the patient’s eyelids open. Drip the tetracaine or saline down the strip and allow it to drip into the eye, being careful to avoid touching the strip to the eye.
Make a fluorescein dropper. This is well detailed in the Tricks of the Trade: Fluorescein application techniques for the eye form Academic Life in Emergency Medicine (link: https://www.aliem.com/2015/06/tricks-of-the-trade-fluorescein-eye/). The Angiocath dropper allows for better control of droplet size and makes it easier to instill fluorescein into the squinting eye without the risk of touching the cornea.
PEMBlog.com - https://wp.me/p2EBRt-1je
Vimeo.com - https://vimeo.com/287706199
Brad Sobolewski, MD, MEd
Associate Professor, Assistant Director - Pediatric Residency Training Program
Division of Emergency Medicine
Cincinnati Children's Hospital Medical Center
How To Cite This Post
[Peer-Reviewed, Web Publication] Richardson J, Moore A. (2019, May 20). Corneal Abrasions [NUEM Blog. Expert Commentary by Sobolewski]. Retrieved from http://www.nuemblog.com/blog/corneal-abrasion
Other Posts You May Enjoy
References
Images courtesy of http://www.tedmontgomery.com/the_eye/
Marx, J. A., & Rosen, P. (2014). Rosen's emergency medicine: Concepts and clinical practice (8th ed.) Ch. 71. Opthamology. Philadelphia, PA: Elsevier/Saunders
Yanoff, M., Duker, J. S., & Augsburger, J. J. (2009). Ophthalmology. Ch 4, Corneal anatomy, physiology, and wound healing. Edinburgh: Mosby Elsevier.
Roberts, J. R., In Custalow, C. B., In Thomsen, T. W., & In Hedges, J. R. (2014). Roberts and Hedges' clinical procedures in emergency medicine. Ch 62. Opthalmologic procedures.
Gardiner, M. F. Overview of eye injuries in the emergency department. Retrieved September 16, 2017, from https://www.uptodate.com/contents/overview-of-eye-injuries-in-the-emergency-department.
Jacobs, D. S. Corneal abrasions and corneal foreign bodies: management. Retrieved September 16, 2017, from https://www.uptodate.com/contents/corneal-abrasions-and-corneal-foreign-bodies-management.
Waldman, N., Winrow, B., Denise, I., Gray, A., McMAster, S., Giddings, G., & Meanley, J. (2017). An observational study to determine whether routinely sending patients home with a 24-hour supply of topical tetracaine from the emergency department for simple corneal abrasion pain is potentially safe. Annals of Emergency Medicine, 02(016).
Canthotomy
Written by: Alex Ireland, MD (NUEM PGY-3) Edited by: Gabrielle Ahlzadeh, MD (NUEM PGY-4) Expert commentary by: Gary Lissner, MD
Expert Commentary
The author has written an excellent illustrated review of the technique of lateral canthotomy and cantholysis for traumatic orbital compartment syndrome due to a significant retrobulbar hemorrhage. As with any procedure it is crucial to understand the indications and contraindications of the procedure. In these cases, the indication is the saving or restoring of vision lost due to excessive intraorbital pressure, and the contraindication is generally an opened globe. This is a difficult situation because there is usually limited information and there is a limited amount of time to relieve the orbital compartment syndrome. The timing of the onset of the retrobulbar hemorrhage that created the critical pressure to cause loss of vision is often unknown. The decision to decompress is usually based solely on a clinical examination without having time to obtain orbital radiologic studies and before an ophthalmologist can arrive to evaluate the patient. However, the clinical exam could be limited if the patient is not cooperative or is not conscious.
Initially a determination has to be made if the globe is lacerated or ruptured which could preclude the performance of the canthotomy and cantholysis . Either a ruptured globe or an orbital compartment syndrome can cause loss of vision. A ruptured globe can occur along with a retrobulbar hemorrhage. If the eyeball is opened, no additional external pressure should be placed on the lids or globe in order to prevent additional damage to the eye. An opened globe could be determined by seeing a laceration of the globe, seeing protruding intraocular contents, finding a very soft eye, and/or finding a distorted eye. If the eyeball is opened, a sturdy shield should be placed resting on the surrounding orbital bone to protect the eye from external pressure, and the aide of an ophthalmologist should be sought.
If it is determined that the globe is intact, a decision has to be made on clinical examination findings if a significant retrobulbar hemorrhage exists that would create enough pressure in the orbit to cause loss of vision. There is usually not enough time to wait for imaging studies to be done. The trauma could create a large enough orbital fracture that could decompress the orbital pressure and the orbital compartment syndrome. On the other hand, an orbital fracture can create orbital emphysema. Blowing of the nose by the patient can increase the emphysema and further increase the intraorbital pressure, creating a sight-threatening orbital compartment syndrome.
Acute vision loss is the key clue to a significant orbital compartment syndrome, but many trauma patients may not be able to cooperate for visual testing. The reaction of the pupil to light can be used as a sign of visual loss even in the uncooperative patient. With an orbital compartment syndrome, the pupil of the involved eye will not react well to a bright light and will have an afferent defect. However, if the patient was given narcotics the pupils can become miotic and pupil testing becomes difficult. Visual loss is not diagnostic of an orbital compartment syndrome because the trauma can create other damage that can cause visual loss including intraocular bleeding, retinal disorders, traumatic optic neuropathy, or a lacerated or ruptured globe. Trauma can cause edema and ecchymosis of the lids, but tense proptosis with very firm retropulsion of the involved eye is a key diagnostic finding of a significant retrobulbar hemorrhage. As the orbital bleeding continues, the eye is pushed forward against the tight eye lids and the intraocular pressure increases. A significant intraocular pressure increase can be used as another sign of an orbital compartmental syndrome. Checking the intraocular pressure can be difficult in the presence of massive eyelid swelling. Pulling the lids opened especially if the patient is squeezing can transmit the external pulling pressure to the eye, creating a false reading of a raised intraocular pressure. Using curved instruments, or the blunt end of bent paper clips as shown by the Blog’s author, can help open the lids. Using a topical anesthetic to reduce eye discomfort, or using injectable local anesthetic to relax the orbicularis muscle action can also help to more easily open the eyelids to obtain a more accurate intraocular pressure. Orbital compartment syndrome will limit extraocular motility on the involved side, but the unconscious patient’s motility cannot be easily tested. A significant increase of the orbital pressure and the intraocular pressure can cause pulsation of the retina arteries and full retina veins which can help with the diagnosis of an orbital compartment syndrome if the fundus is viewed.
The Blog gives a precise pictorial and written description of the lateral canthotomy and cantholyisis technique. However, unlike the author’s demonstration photos, most cases with significant traumatic orbital compartment syndrome have massive lid ecchymosis and subconjunctival hemorrhage and a proptotic eye that is pushed forward tightly against the lids. Therefore, there is frequently little room to insert the instruments at the lateral canthal angle. Extreme care must be taken to avoid unwanted damage. The author’s “tip” to insert a Morgan lens (a sclera shell if available can also be used) onto the patient’s eye is a good idea to help protect the eye, but the tight space in some cases can prevent the insertion of the lens. It is important that when working in the tight space to always work with the instruments pointing away from the eye and orbit to prevent injury to the globe, lateral rectus, lacrimal gland, or deeper orbital tissues. Always aim anteriorly toward the anterior orbital boney rim during the canthotomy. As the author suggests, the lids should be pulled or lifted away from the eyeball. Pulling the eyelid nasally and anteriorly helps tighten the crus of the lateral canthal tendon, thus making it easier to feel or strum the crus and cut it during the cantholysis. Always keep the tip of the scissors pointed away from the globe.
An orbital compartment syndrome can also occur with retrobulbar hemorrhage after surgery in the region. In such cases it can be advisable to first open the surgical wounds to determine if release of blood and clots from the depths of the wounds relieves the problem and thus eliminating the need for the canthotomy and cantholysis. In cases of retrobulbar hemorrhage after sinus or nasal surgery, the removal of nasal or sinus packing could release the blood and relieve the orbital compartment syndrome.
The Blog’s author presents a good list of potential complications from the canthotomy and cantholysis procedure. Many of the patients with significant retrobulbar hemorrhage are elderly patients who fall on their face. This group of patients can be on anticoagulants that could have potentiated the initial orbital hemorrhage and could create a problem of continued bleeding. The patients have to be observed after the canthotomy and cantholysis for continued or recurrent orbital bleeding and also for the possibility of a newly created surgical site eyelid bleeding that may not stop spontaneously. Additional surgery could be needed to stop the bleeding. Also to be considered as a complication is the fact that the release of the lateral canthal tendon lid support could cause lower lid ectropion, lid retraction, or lateral canthal deformity. Such deformities sometimes have to be surgically repaired.
In conclusion, the author has written a Blog which gives an excellent guide to perform a canthotomy and cantholysis. It can be difficult to make the decision if the procedure is needed to be done to prevent permanent loss of vision of an eye. The decision has to be based on clinical examination findings and the procedure if needed should not be delayed. After the procedure the patient needs to be observed and to have an evaluation by an ophthalmologist.
Gary S. Lissner, MD
Associate Professor, Chief Ophthalmic Plastics Service, Department of Ophthalmology, Northwestern University Feinberg School of Medicine
References
Yung CW, Moorthy RS, Lindley D, Ringle M, Nunery WR. Efficacy of lateral canthotomy and cantholysis in orbital hemorrhage. Ophthalmic Plast Reconstr Surg. 1994 June; 10(2):137-41.
Lima V, Burt B, Leibovitch I, Prabhakaran V, Goldberg RA, Selva D. Orbital compartment syndrome: the ophthalmic surgical emergency. Surv Ophthalmol. 2009 Jul-Aug; 54(4): 441-9.
Kent TL, Morris CL, Scott IU, Fekrat S. Evaluation and management of orbital hemorrhage. Eye Net magazine. 2018 July.
Jaksha AF, Justin GA, Davies BW, Ryan DS, Weichel ED, Colyer MH. Lateral canthotomy and cantholysis in operations Iraqi Freedom and Enduring Freedom: 2001-2011. Ophthalmic Plast Reconstr Surg. 2018 Jul 3. [Epub ahead of print].
How To Cite This Post
[Peer-Reviewed, Web Publication] Ireland A, Ahlzadeh G. (2019, April 15). Canthotomy [NUEM Blog. Expert Commentary by Lissner G]. Retrieved from http://www.nuemblog.com/blog/canthotomy
Other Posts You May Enjoy
Optic Neuritis
Written by: Steve Chukwulebe, MD (NUEM PGY-4) Edited by: Victor Gappmaier, MD (NUEM Alum ‘18) Expert commentary by: Shira Simon, MD, MBA
Case:
31-year-old female, with no significant past medical history, presents to the emergency department with a mild headache and blurry, decreased vision in the right eye for the past 2 days. Other historical elements include that the patient has been experiencing pain with eye movement. However, she denies difference in color perception. She also denies any trauma to the eye, recent fevers, chills, malaise, exposures, or travel. The left eye is unaffected.
Exam:
Normal vitals and a well appearing female of stated age
Ocular exam reveals normal appearing eyes without chemosis, proptosis, conjunctival injection, scleritis, icterus, or foreign bodies
Non-dilated funduscopic exam is unremarkable
Visual acuities are OD: 20/40 and OS: 20/20
Tonometry reveals right and left eye pressures are < 20 mmHg
Slit lamp exam is without cells or flare
Fluorescein stain is without any corneal uptake
CN 3-12 are intact, and no focal neurologic deficits on exam
Differential Diagnosis [1,2]:
Painless Vision Loss
Central retinal artery occlusion
Central retinal vein occlusion
Retinal detachment
Vitreous detachment/vitreous hemorrhage
Tumor/Mass
Stroke
Painful Vision Loss
Acute angle closure glaucoma
Scleritis
Anterior uveitis (iritis)
Optic neuritis
Keratitis
Corneal abrasion/trauma
Temporal arteritis
The challenge in diagnosing optic neuritis is to exclude other causes of acute monocular vision loss. Therefore, a normal appearing eye, slit lamp exam, fluorescence stain, and intraocular pressures eliminates scleritis, uveitis, keratitis/abrasion, and glaucoma respectively [5]. Additionally, the history is less suggestive of other urgent and emergent ocular pathologies such as retinal detachment and central retinal artery occlusion.
Some physical exam findings more specific to optic neuritis include:
Afferent pupillary defect
Optic disk swelling and papilledema, which can be seen by ultrasound [6]
Decreased perception in the saturation of deep red colors
Decreased visual acuities ranging from 20/25 to 20/190, and even no light perception[4]
Eye pain, especially with eye motion, is seen in 92 percent of patients
Loss of color vision out of proportion to the decrease in visual acuity
Retro-orbital headache
Further diagnostics may include an MRI of the brain and orbits, but is not necessary for the diagnosis of optic neuritis [5]. MRI can help characterize the disease burden and assess the risk for the development of multiple sclerosis [7].
Given the patient’s age and constellation of symptoms, both neurology and ophthalmology consultation were performed with the leading concerning diagnosis being optic neuritis. The patient was admitted for further evaluation with a dilated ocular exam, MRs of the brain, and treatment.
Pathophysiology and Clinical Disease:
Optic neuritis is an inflammatory and demyelinating process that usually presents with monocular vision loss [3-4]. While there are many causes for optic neuritis, the demyelinating lesions seen in optic neuritis are similar to those that have been associated with multiple sclerosis. Patients are typically women between the ages of 20-40. Patients often develop progressive symptoms over a period of a few hours to several days.
Treatment and Timing:
Typical treatment is high dose intravenous steroids for three days. Another treatment regimen that has been described is intravenous methylprednisolone (250 mg four times per day) for three days, followed by oral prednisone (1 mg/kg per day) for 11 days, and then a four-day taper [8, 9].
If the diagnosis is uncertain, then is it acceptable to delay treatment for an MRI or specialist consultation the following morning?
The Optic Neuritis Treatment Trial described treatment of optic neuritis with high dose intravenous methylprednisolone. The initial multicenter trial enrolled 457 patients from July 1, 1988, through June 30, 1991. They ultimately randomized 389 patients with acute optic neuritis (and without known multiple sclerosis) to receive intravenous methylprednisolone (250 mg every six hours) for 3 days followed by oral prednisone (1 mg per kilogram of body weight) for 11 days, oral prednisone (1 mg per kilogram) alone for 14 days, or placebo for 14 days. They then assessed the neurologic status of the subjects for a period of two to four years and published their results in 1993. Also by following the subjects longitudinally, the authors were able to reanalyze the data and publish again in 2003. From the initial study, it was learned that high the steroids hastened the recovery of visual function, but did not affect long term visual outcomes when compared to both placebo and oral prednisone [10, 11, 12] after six months, and ten-year follow-up. It was found that a 3-day course of methylprednisolone reduced the rate of development of multiple sclerosis over a 2-year period [12]. Multiple sclerosis developed within the first two years in 7.5 percent of the IV methylprednisolone group vs. 14.7 percent of the oral prednisone group vs. 16.7 percent of the placebo group. The adjusted rate ratio for the development of definite multiple sclerosis within two years in the intravenous methylprednisolone group was 0.34 as compared with the placebo group and 0.38 as compared with the oral-prednisone group. However, after a 5-year period the treatment effect was no longer significant for the same group of patients.
Therefore, in a scenario when a provider may delay high dose steroids for a neurology and ophthalmology consultation, or for an MRI, it can be inferred that this delay will not affect long term outcomes for the patient. However, given that early treatment hastens symptom recovery and delays progression to multiple sclerosis, it may be beneficial to start high dose IV steroids in the emergency department in patients if optic neuritis is the suspected diagnosis.
Expert Commentary
This is a very good review of optic neuritis. There are just a few, additional nuanced points I’d like to mention, as well as some tips on counseling the patient.
Visual field changes: A central visual field deficit is commonly seen with this entity. It is most easily detected on formal visual field testing in the ophthalmology clinic (Humphrey or Goldmann visual fields), though some patients may report this on their own in the acute care setting.
Optic nerve swelling: In the ONTT, only 35% of patients had disc swelling (65% had normal appearing optic nerve heads on fundoscopy), so evaluating with ultrasound would not be revealing in most cases.
MRI for diagnosis: MRI is actually very important for the diagnosis of optic neuritis, as inflammation of a different part of the optic nerve (other than the nerve head) can only be visualized radiographically. MRI of the orbits and brain should be obtained with thin slices through the orbits, with fat suppression, and gadolinium (in addition to FLAIR sequences to look for demyelination).
Differential diagnosis: While this article talks about optic neuritis from demyelination related to possible MS, it’s important to bear in mind that there are other causes of optic neuritis: autoimmune disease (e.g., lupus), infections (e.g., syphilis or Lyme), other inflammatory conditions (e.g., sarcoidosis), other demyelinating processes (like neuromyelitis optica), or it can be idiopathic.
When counseling the patient about prognosis, it may be helpful to remember the “10-20-40-60” rule. I had been taught this, and it helps quickly summarize the ONTT prognostic statistics (that are outlined very nicely in this article). The “10-20-40-60 rule” mnemonic reminds us that at 10 years: there is a 20% chance of developing MS after an episode of idiopathic optic neuritis if there were no white matter lesions found on MRI; a 40% chance regardless of MRI findings; and, a 60% chance if 1+ white matter lesions are found on MRI.
It is also helpful to let the patient know that visual recovery is often excellent. Most patients return fairly close to their baseline vision within 3-5 weeks, although they may note some lingering difficulties with contrast sensitivity and color vision. An afferent pupillary defect may also persist.
Shira Simon, MD, MBA
Assistant Professor of Ophthalmology and Neurology
Northwestern Medicine
How to Cite This Post
[Peer-Reviewed, Web Publication] Chukwulebe S, Gappmaier V. (2019, March 11). Optic Neuritis. [NUEM Blog. Expert Commentary by Simon S]. Retrieved from http://www.nuemblog.com/blog/optic-neuritis
Other Posts You May Enjoy
Resources
Dargin JM, Lowenstein RA. The painful eye. Emerg Med Clin North Am. 2008;26(1):199-216, viii.
Vortmann M, Schneider JI. Acute monocular visual loss. Emerg Med Clin North Am. 2008;26(1):73-96, vi.
The clinical profile of optic neuritis. Experience of the Optic Neuritis Treatment Trial. Optic Neuritis Study Group. Arch Ophthalmol. 1991;109(12):1673-8.
UpToDate
Germann CA, Baumann MR, Hamzavi S. Ophthalmic diagnoses in the ED: optic neuritis. Am J Emerg Med. 2007;25(7):834-7.
Teismann N, Lenaghan P, Nolan R, Stein J, Green A. Point-of-care ocular ultrasound to detect optic disc swelling. Acad Emerg Med. 2013;20(9):920-5.
Beck RW, Arrington J, Murtagh FR, Cleary PA, Kaufman DI. Brain magnetic resonance imaging in acute optic neuritis. Experience of the Optic Neuritis Study Group. Arch Neurol. 1993;50(8):841-6.
Beck RW, Cleary PA, Anderson MM, et al. A randomized, controlled trial of corticosteroids in the treatment of acute optic neuritis. The Optic Neuritis Study Group. N Engl J Med. 1992;326(9):581-8.
Sellebjerg F, Nielsen HS, Frederiksen JL, Olesen J. A randomized, controlled trial of oral high-dose methylprednisolone in acute optic neuritis. Neurology. 1999;52(7):1479-84.
Beck RW, Gal RL, Bhatti MT, et al. Visual function more than 10 years after optic neuritis: experience of the optic neuritis treatment trial. Am J Ophthalmol. 2004;137(1):77-83.
Beck RW, Trobe JD, Moke PS, et al. High- and low-risk profiles for the development of multiple sclerosis within 10 years after optic neuritis: experience of the optic neuritis treatment trial. Arch Ophthalmol. 2003;121(7):944-9.
Beck RW, Cleary PA, Trobe JD, et al. The effect of corticosteroids for acute optic neuritis on the subsequent development of multiple sclerosis. The Optic Neuritis Study Group. N Engl J Med. 1993;329(24):1764-9.
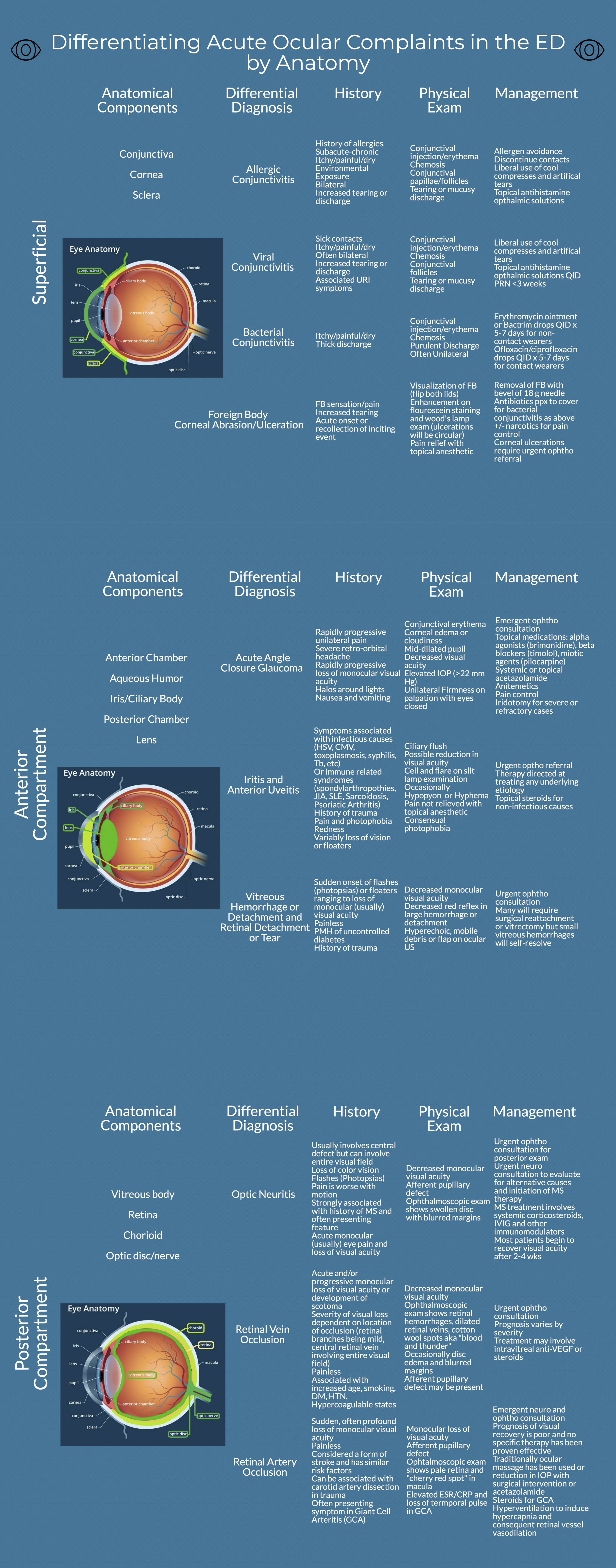
Anatomic Approach to Ocular Complaints
Written by: Philip Jackson, MD (NUEM PGY-3) Edited by: Jesus Trevino, MD (NUEM PGY-4) Expert commentary by: Rehan Hussain, MD
Expert Commentary
Thank you for this excellent diagram, which demonstrates a thorough and systematic approach to the most common ocular complaints one would encounter in the ED. In assessing a painful red eye, there is so much value in determining whether the discomfort is relieved with topical anesthetics, as you can reliably confine the pathology to the cornea or conjunctiva in those cases. However, a red eye associated with deep achy pain that is not relieved with tetracaine could be caused by scleritis, which is highly associated with autoimmune disease. If cells and flare are visible in the anterior chamber, uveitis is more likely. Any history of a recent eye procedure should prompt you to consider endophthalmitis, which can be visually devastating, and warrants urgent ophthalmology referral.
In diagnosing conjunctivitis, you did a great job of highlighting the importance of a good history in determining the etiology . I would add that asking about sexual history can be valuable, as gonorrhea can present with copious purulent discharge, and chlamydia can present with chronic follicular conjunctivitis. Both would warrant systemic antibiotics and treatment of partners, in addition to eyedrops.
Acute angle closure glaucoma is a diagnosis that should be considered in almost all cases of unilateral headache. It can mimic migraine, since both may present with nausea, vomiting, and visual disturbances. Checking the eye pressure is the most important step to making the diagnosis.
Finally, acute onset of floaters and/or flashes always warrants an ophthalmology consult to rule out retinal detachment. Ultrasound is a useful tool to differentiate retinal detachment from posterior vitreous detachment (PVD) and vitreous hemorrhage. PVD and vitreous hemorrhages tend to move freely when the eye moves, whereas retinal detachment is anchored to the nerve but still flaps with eye movement.
Once again, this diagram serves as a very helpful flowchart to trouble-shoot eye complaints in the ED.
Rehan M. Hussain, MD
Vitreoretinal Surgery Fellow
Bascom Palmer Eye Institute
University of Miami Health System
How To Cite This Post
[Peer-Reviewed, Web Publication] Jackson P, Trevino J (2018, October 22). Anatomic approach to ocular complaints. [NUEM Blog. Expert Commentary by Hussain R]. Retrieved from http://www.nuemblog.com/blog/ocular-complaints
Other Posts You May Enjoy
Open Globe Injury
Written by: Justine Ko, MD (NUEM PGY-1) Edited by: Hashim Zaidi, MD (NUEM PGY-3) Expert commentary by: Rehan Hussain, MD
Expert Commentary
Hi Drs. Ko & Zaidi,
Thank you for this great review on emergency management of open globe injuries. The presentation of open globe injuries can vary widely depending on the mechanism of injury, and so can the final visual outcome. For obvious ruptured globes with peaked pupils or extruding intraocular contents, I am glad you emphasized that it is best to avoid any manipulation of the eye to prevent further extrusion of contents or increase the risk of infection. Cover the eye with a shield, start topical and systemic antibiotics, and consult ophthalmology so they can arrange surgery in a timely manner. The patient must be kept NPO to avoid delaying surgery unnecessarily. Definitely don’t check the eye pressure if you already know it is a ruptured globe.
For the less obvious ruptured globes, which may sometimes mimic a corneal or conjunctival abrasion, it is imperative to perform a Seidel test carefully. This involves placing a wet fluorescein strip (not the pre-made drop) over the suspected entry site, looking at it under the cobalt blue light of the slit lamp, and checking to see if a stream of aqueous fluid is coming out of the injury site (it can be either quick or a slow stream). Fluorescein staining in absence of a stream of fluid indicates that only an abrasion is present. When in doubt, consult ophthalmology for confirmation. Other slit lamp findings that may be present include subconjunctival hemorrhage, chemosis, corneal abrasion, hyphema, flat anterior chamber, iris defects, foreign body in the anterior chamber, or traumatic cataract.
For imaging workup, CT of the ORBITS is preferable, as it allows for 1 mm sections that increase the likelihood of detecting small intraocular foreign bodies (IOFB) that might be missed with a standard head CT. MRI should be avoided as it is slow, costly, and can cause movement of metallic IOFBs, causing further damage to the eye. Gentle ultrasound over the closed eyelids could be used in absence of availability of CT, but I prefer to avoid it since puts pressure on the eye.
The patient and family members are often times distraught over the injury, and appropriate counseling is an essential part of the encounter. They frequently ask if they will be permanently blind. I avoid making any predictions on the final visual outcome, as it is difficult to predict and can lead to either unmet expectations or unnecessary anxiety. I say that the goal is to save the eye at this time, and we will follow closely to see how the vision turns out. Sometimes patients do very well if the extent of injury is not severe, but on other occasions patients require multiple surgeries to correct associated retinal detachment, vitreous hemorrhage, or lens dislocation. If appropriate antibiotic therapy is not initiated, there is an increased risk of developing endophthalmitis, which portends a poor visual prognosis.
Rehan Hussain, MD
Vitreoretinal Surgery Fellow, Bascom Palmer Eye Institute, Univeristy of Miami
Posts You May Also Enjoy
How to cite this post
[Peer-Reviewed, Web Publication] Ko J, Zaidi H (2018, Feb 26). Open Globe Injury. [NUEM Blog. Expert Commentary By Hussain R]. Retrieved from http://www.nuemblog.com/blog/globe-rupture.
Resources
Alteveer, J and Lahmann B. 2010. “An Evidence-Based Approach To Traumatic Ocular Emergencies.” Emergency Medicine Practice, 12(5): 1-24. 2017.
“Emergency Management of Traumatic Eye Injuries | 2001-07-01 | AHC Media: Continuing Medical Education Publishing.” 2017. Accessed October 6. https://www.ahcmedia.com/articles/71714-emergency-management-of-traumatic-eye-injuries.
Guluma K, Lee JE. Ophthalmology. In: Gausche-Hill M, Hockberger R, Walls R, eds. Rosen’s Emergency Medicine: Concepts and Clinical Practice. 9th ed. Philadelphia, Pa: Elsevier, Inc. 2018:790-819.e3.
Bord, Sharon P., and Judith Linden. 2008. “Trauma to the Globe and Orbit.” Emergency Medicine Clinics of North America, Ophthalmologic Emergencies, 26 (1): 97–123. doi:10.1016/j.emc.2007.11.006.
“Trauma: Open-Globe Injuries.” 2015. American Academy of Ophthalmology. November 4. https://www.aao.org/pediatric-center-detail/open-globe-injuries.
Harlan JB, Pieramici DJ. Evaluation of patients with ocular trauma. Ophthalmol Clin N Am. 2002;15:153-161. (Review article)
Ahmed, Y, A M Schimel, A Pathengay, M H Colyer, and H W Flynn. 2012. “Endophthalmitis Following Open-Globe Injuries.” Eye 26 (2): 212–17. doi:10.1038/eye.2011.313.
Arey, Mark L., V. Vinod Mootha, Anthony R. Whittemore, David P. Chason, and Preston H. Blomquist. 2007. “Computed Tomography in the Diagnosis of Occult Open-Globe Injuries.” Ophthalmology 114 (8): 1448–52. doi:10.1016/j.ophtha.2006.10.051.
A Visual Guide to Acute Angle Closure Glaucoma
Glaucoma is one of the leading causes of preventable blindness. While most cases are due to chronic open-angle glaucoma, acute angle-closure glaucoma is an ophthalmic emergency. This week we present a visual guide to successful management of these patients in the emergency department.
Color Coded Clarity
The American Academy of Ophthalmology (AAO) has been attempting to reduce errors in ophthalmic drops since the mid-90’s with the advocacy of a uniform color coded system for topical ocular medications. This standardized color system would then theoretically help patients and providers identify medications correctly and reduce errors both inpatient and outpatient.





































What should you do for patients who fall victim to riot control agents?