Written by: Laurie Aluce, MD (NUEM PGY-3) Edited by: Kimberly Iwaki MD (NUEM Alum ‘18 ) Expert commentary by: Daniel Schimmel, MD
The Case:
Patient: 57 year old male
Chief Complaint: Chest Pain
PMH: Hypertension
Pain: Mid-sternal, non-radiating, 6/10, constant pressure
Onset: 45 minutes ago while watching TV
Associated symptoms: No diaphoresis, light-headedness, nausea, vomiting, or back pain
Vitals: T 98.8, HR 70, BP 110/68, RR 14, Sat 100% on room air
Physical Exam:
General: Alert, no apparent distress, sitting comfortably in cart
Cardiac: Regular rate and rhythm, no murmurs/rubs/gallops
Pulmonary: Clear to auscultation bilaterally, no crackles/wheezes
Extremities: Warm and well perfused, 2+ distal pulses, cap refill < 2s
Labs: In process
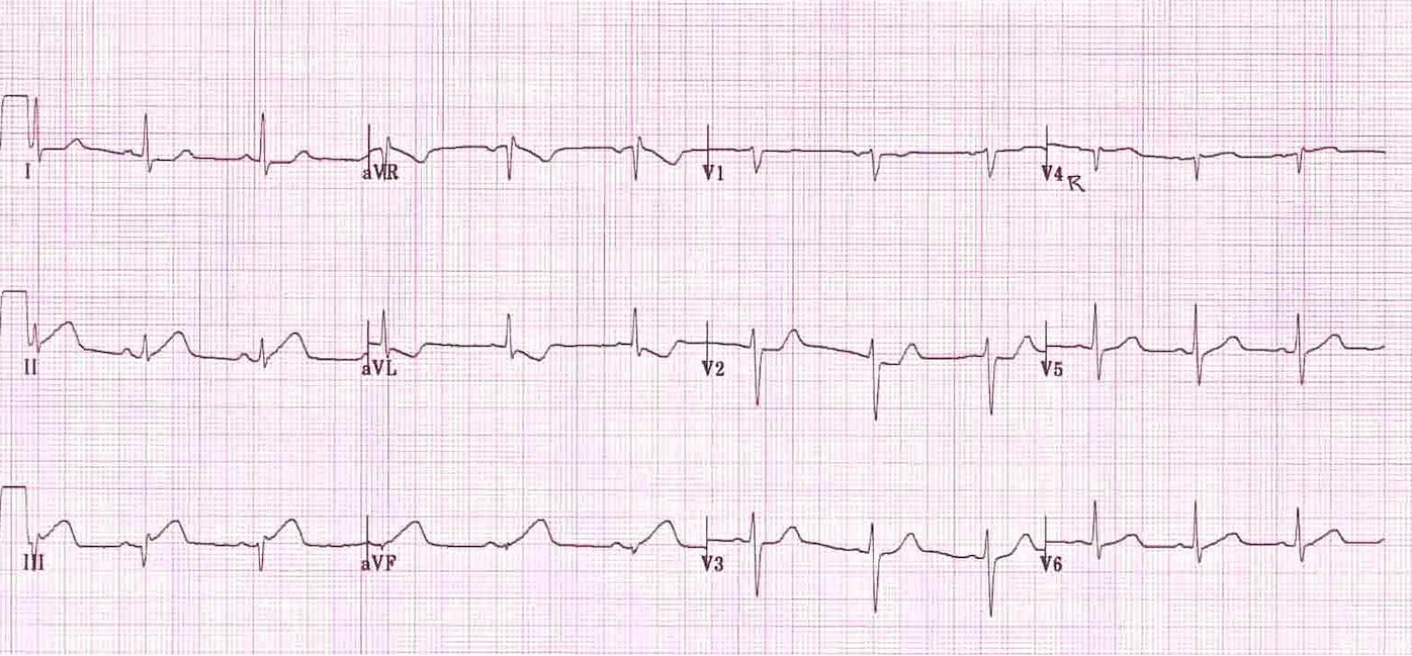
Triage EKG:
Image from Stephen Smith, MD. http://hqmeded-ecg.blogspot.com/2011/02/inferior-hyperacute-t-waves-clue-is-t.html
What abnormalities do you see in this EKG?
Prolonged PR interval
Slightly widened QRS
Hyperacute T waves in II, III, aVF
T wave inversion (TWI) in aVL
< 1mm ST depression in I, avL
What are you concerned about? What elements of this EKG raise your concern?
Inferior myocardial infarction (MI) due to hyperacute T waves in II, III, aVF
Inferior MI or significant mid left anterior descending (LAD) lesion due to TWI in aVL [3]
How will you differentiate an inferior MI from a chronic mid LAD lesion?
Clinical picture and a repeat EKG. If the TWI is due to a chronic mid LAD lesion, it should not change on serial EKGs. If the TWI is due to an inferior MI, you may see it evolve to ST depression in aVL and/or ST elevation in II, III, aVF. [3]
You obtain a repeat EKG with one right-sided lead, V4R:
Image from Edward Burns, MD. https://lifeinthefastlane.com/ecg-library/basics/inferior-stemi/
What abnormalities do you see in the repeat EKG?
Hyperacute T waves and ST elevation in II, III, aVF
ST depression and TWI in aVL
ST depression in V2
<1mm ST depression in I
<1mm ST elevation in V4R
What are you concerned about? What elements of this EKG raise your concern?
Concern for inferior MI
ST elevation in II, III, aVF
ST depression and T wave inversion in aVL
EKG sensitivity for inferior MI increases from 60% to 77% when criteria includes ≥ 1mm reciprocal ST depression in aVL in addition to ≥ 1mm ST elevation in II, III, aVF [1]
Concern for right ventricle (RV) involvement
25% – 53% of inferior MIs have RV involvement [5]
ST elevation in III > II
Isoelectric ST segment in V1 with ST depression in V2
ST depression and T wave inversion in aVL
>1mm ST depression in aVL has sensitivity of 87% and positive predictive value of 90% for RV involvement with acute inferior MI [5]
Other findings suggestive of RV involvement not pictured in this EKG
ST elevation in V2 > 50% the magnitude of ST depression in aVF [4]
Right bundle branch block, 2nd and 3rd degree AV block
ST elevation in V1
How can your further evaluate for RV involvement?
You ask for a right-sided EKG to check for ST elevation in V3R-V6R, but your EKG tech doesn’t remember where to place the leads. The tech looks to you for help. Where do you put the leads?
Full Right-Sided EKG Standard EKG with V4R
Images from Tom Bouthillet. http://www.ems12lead.com/2008/10/17/12-lead-ecg-lead-placement-diagrams/
If you don't have the time to perform a full right-sided EKG, you can perform a standard EKG but switch V4 to V4R as shown with the prior EKG. V4R is considered the best single lead for diagnosing a right ventricular MI.[2] ST elevation ≥ 1 mm in V4R has a sensitivity of 88% and a specificity of 78% for RV infarction. [6]
EKG with V4R-V6R:
Image from Ary Goldberger, MD. UpToDate: Electrocardiogram in the diagnosis of myocardial ischemia and infarction
What abnormality do you see in the right-sided leads?
ST elevation in V4R-V6R
What is your diagnosis?
Inferior MI with RV infarction
Take Home Points:
Don’t forget aVL. T wave inversion and ST depression in aVL can be a marker of serious cardiac pathology:
Significant mid-LAD lesion
Evolving inferior MI and possible RV involvement
If you are concerned for inferior ischemia, obtain a right-sided EKG to evaluate for right ventricular involvement
Expert Commentary
This is an excellent review of aVL, an important lead for diagnosis and prognosis. Because it can be a modifier, or is used in conjunction with other criteria for diagnosis, it often gets overlooked.
In the acute setting, aVL can be used to help identify ST elevation myocardial infarction (STEMI) in various locations. In addition to the aforementioned use in identifying RV involvement in inferior STEMI and mid LAD lesions, aVL is considered a high lateral lead which is fed by diagonal vessels. As such, acute blockages that affect the proximal LAD with anterior STEMI in V3, V4, anteroseptal involvement in V1, V2 and may also have high lateral involvement in aVL. While I am always watching for shock and unstable arrhythmias taking patients to the cardiac catheterization lab, if I see this distribution with an anterior STEMI, I am even more concerned due to the amount of myocardium subtended by the lesion. I often preemptively get access for cardiac mechanical support in case cardiogenic shock develops. In this way, the prognostic information from aVL may change practice in the cardiac catheterization lab.
Not to be overlooked, leads I and aVL may be the only leads with ST elevation in an isolated high lateral STEMI in a diagonal vessel. Diagonal 1 or diagonal 2 may be large vessels and be the only vessel with acute thrombosis. aVL is the reciprocal lead to the inferior leads in inferior STEMI. Similarly, lead III may move reciprocally, showing ST segment depression in the high lateral STEMI with elevation in aVL.
As nice as it can be to have aVL to prognosticate inferior STEMI, prognosticate anterior STEMI and identify isolated high lateral STEMI, aVL ST segments and T waves can be abnormal for non-acute reasons leading to a lack of specificity. The most common reason for an abnormal repolarization in aVL is strain in the setting of LVH. So how do we differentiate acute reciprocal changes from strain pattern?
A frequently overlooked bit of information on the EKG is the QRS-T angle. Luckily this is reported for us on the EKG at the top. In the setting of T wave inversion, if the angle is greater than 100 degrees, this is more consistent with strain. Furthermore, if the ST segment leading to the T wave is downwardly concave (think downward parabolic curve) with asymmetry of the T wave, this also is more consistent with strain. If we look at the presented case’s EKGs, we can dissect them a bit further. In the triage EKG, there isn’t ST segment depression at all. In fact there is elevation with a T wave inversion. This is concerning. The ST segment may be isoelectric with an inverted T wave, but there should not be ST elevation with a T wave inverted in the opposite direction. This morphology is often used in Sgarbossa criteria to identify STEMI in left bundle branch block. So in addition to the hyperacute T waves of this triage EKG, aVL is very concerning. In the follow-up EKG, we can see dynamic changes that have occurred in the inferior leads solidifying the diagnosis. But aVL also suggests RV involvement. The ST segment is downsloping, depressed without concavity (more linearly pointing down to the right). To clinch the diagnosis of RV involvement, we also see the right sided leads with elevation.
It is definitely possible to have a patient with LVH/strain findings and also have an acute inferior STEMI. As demonstrated successfully in this case, the statement about serial EKGs is a critical one. Even in the setting of a normal EKG, a good story for myocardial infarction should prompt a serial EKG and often a posterior EKG to identify a supposedly electrocardiographically silent STEMI. Remember STEMI is an EKG diagnosis that is supposed to correlate with the physiologic condition of an acute 100% occlusion of a vessel. In the early period, there can be stuttering pain with opening and closing of the vessel and the EKG may not capture it in that moment or may miss the posterior STEMI if the posterior EKG is not obtained.
To sum up the importance of aVL:
Inferior STEMI: Improved diagnosis when aVL has a depressed ST segment with an inverted T wave
Inferior STEMI: Considered worse prognosis when aVL has a depressed ST segment with an inverted T wave as it suggests a more proximal RCA occlusion with RV involvement. ST elevation in V1 or right sided V4 may also be helpful in identifying proximal RCA occlusion with RV branch involvement.
Anterior STEMI: aVL STEMI confers a worse prognosis, suggesting more proximal LAD involvement.
Isolated high lateral STEMI: ST elevation in leads I and aVL may identify an acute 100% blockage in a diagonal vessel. Lead III may have reciprocal ST segment depression.
To differentiate strain from ischemic changes in aVL:
QRS-T angle: If greater than 100, may be consistent with strain.
ST segment slope: If concave, consider strain. If downsloping but the ST segment is more straight as it aims downward, consider an acute event.
T Wave inversion: If there is asymmetry to the inverted T wave, it may be more consistent with strain.
In summary, the EKG has so much data in it. Pattern recognition can be a wonderful tool for quick diagnosis of clear problems. But a methodical evaluation of the EKG can still be done quickly and identify what others may miss.
Dr. Daniel R. Schimmel
Assistant Professor of Medicine
Bluhm Cardiovascular Institute
Northwestern University
References:
1. Birnbaum Y, et al. ST segment depression in aVL: a sensitive marker for acute inferior myocardial infarction. Eur Heart J 1993;14(1):4-7.
2. Carley SD. Beyond the 12 lead: Review of the use of additional leads for the early electrocardiographic diagnosis of acute myocardial infarction. Emergency Medicine 2003;15: 143-54.
3. Hassen GW, et al. Lead aVL on electrocardiogram: emerging as important lead in early diagnosis of myocardial infarction. Am J Emerg Med 2014;32(7)785-88.
4. Somers MP, et al. Additional electrocardiographic leads in the ED chest pain patient: right ventricular and posterior leads. Am J Emerg Med 2003;21(7):563-73.
5. Turhan H, et al. Diagnostic value of aVL derivation for right ventricular involvement in patients with acute inferior myocardial infarction. Ann Noninvasive Electrocardiol 2003;8:185-88.
6. Zehender M, et al. Right ventricular infarction as an independent predictor of prognosis after acute inferior myocardial infarction. N Engl J Med 1993; 328:981-88.
How to Cite this Post
[Peer-Reviewed, Web Publication] Aluce L, Iwaki K. (2019, Aug 12). Don’t Forget aVL. [NUEM Blog. Expert Commentary by Schimmel D]. Retrieved from http://www.nuemblog.com/blog/dont-forget-aVL/.
















An engaging and discussion of the severe end of the spectrum of DVT