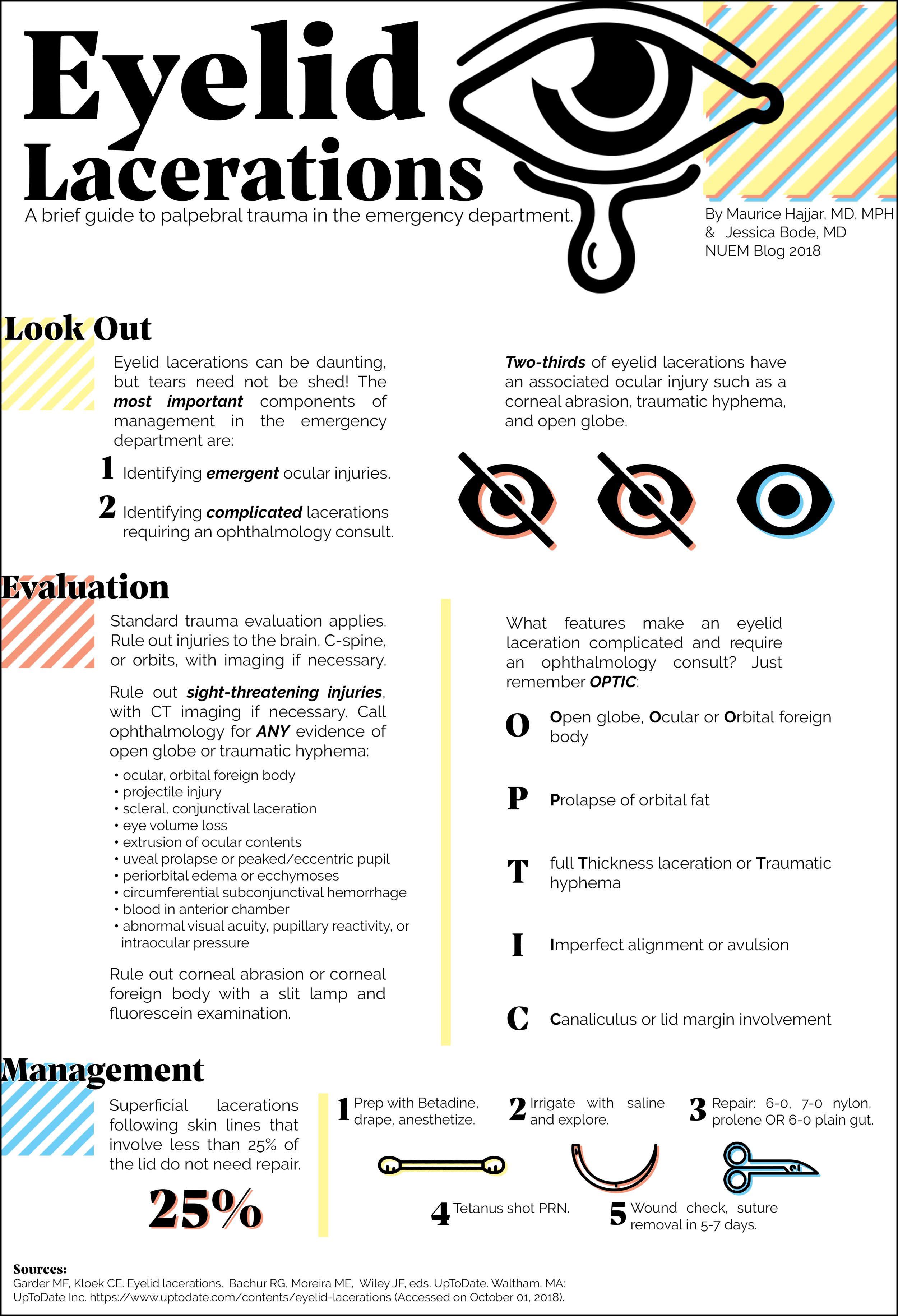
Written by: Maurice Hajjar, MD (PGY-2) Edited by: Jessica Bode, MD (NUEM ‘19) Expert Commentary by: Rehan Hussain
Expert Commentary
Thank you for this excellent diagram, which demonstrates a thorough and systematic approach to eyelid lacerations encountered in the Emergency Room. I have a few extra pearls that may aid ER physicians in management of eyelid lacerations.
Be suspicious in glancing blunt trauma to the cheek or zygoma. This type of blow puts a great deal of stress on the medial canthal anatomy and may result in avulsion of the medial canthus with coexistent canaliculus laceration. This type of laceration may be missed because of the blunt mechanism and because the medial canthal tissues often reappose into a reasonable position, masking the extent of the injury. Look for displacement, excessive rounding, or abnormal laxity of the medial canthus.
Dog bites are notorious for causing canalicular lacerations. Canalicular probing should be performed in all such cases, even with lacerations that appear to be superficial. In some cases, debridement of necrotic tissue is warranted. With uncooperative children, conscious sedation or examination under anesthesia is often necessary to thoroughly examine the eyelids and globes. Administer systemic antibiotics if contamination or foreign body is suspected. For animal bites, consider rabies prophylaxis if warranted. Note that canalicular lacerations are not an ophthalmological emergency and repair can be delayed for 3-7 days without long term negative effects.
Visible orbital fat in an eyelid laceration indicates penetration of the orbital septum, and all such patients require CT imaging and documentation of levator and extraocular muscle function. Exploration of deeper tissue planes may be needed and ophthalmology consultation is warranted. Do not remove any foreign body prior to surgery if there is a possibility of globe penetration or extension into the orbit – this is best performed in a controlled OR environment. A multi-disciplinary approach may be necessary with ophthalmology and possibly ENT or neurosurgery depending on the extent of the injury.
When repairing lacerations, try to not overdo the subcutaneous lidocaine, because it can cause tissue distortion and make the repair more challenging, though you must find a balance to keep the patient comfortable during the repair. It is advisable to place a drop of proparacaine and a protective shell over the eye to prevent any inadvertent globe trauma. I prefer to use absorbable vicryl or gut sutures in children or if the patient seems unlikely to follow up. I enjoy your clever OPTIC mnemonic, and agree all of those listed scenarios should result in an ophthalmology consult.
Rehan M. Hussain, MD
Ophthalmology
Retina Associates, Ltd
How to Cite this Post
[Peer-Reviewed, Web Publication] Hajjar, M, Bode, J. (2020, May 4). Eyelid Lacerations [NUEM Blog. Expert Commentary by Hussain, R]. Retrieved from http://www.nuemblog.com/blog/eyelid-lac