Written by: Melissa Kubacki, MD, MS (NUEM ‘26) Edited by: Jalea Moses, MD (NUEM ‘24)
Expert Commentary by: Matt Levine, MD
Introduction:
Compartment syndrome is a “can’t miss” diagnosis for any painful extremity examination—especially in those with any traumatic mechanism. Having a high clinical index of suspicion along with the skills to accurately measure compartment pressures, while in the emergency department, could save a limb. Accessing compartment pressures by manually palpating the suspected compartment for increased firmness, albeit quick, is largely inaccurate and could cost your patient valuable (and viable) tissue. One study found that diagnosing compartment syndrome on manual palpation alone was only 24% sensitive and 55% specific. This is in comparison to measuring the pressures though the Stryker method which was found to be 94% sensitive and 98% specific. Why risk a missed diagnosis when this method is much simpler and faster than you think?
Indications:
Do you remember “the 6 P’s” of compartment syndrome? There is an easy memory hook, representing key hallmark signs in acute compartment syndrome. In no specific order:
Pain Out of Proportion to Exam
Poikilothermia- thermoregulatory dysregulation, in this case usually a cold limb
Paresthesia
Pallor
Paralysis
Pulselessness
Pain is the key finding; the remainder are late signs that may or may not be present. For example, the presence of a pulse and adequate capillary refill should not rule out evolving compartment syndrome. Maintain your high index of suspicion.
Contraindications:
There are no absolute contraindications to measuring compartment pressures when compartment syndrome is suspected. Some academic sources note a relative contraindication of measuring pressures over a cellulitic site; however, if there are no other insertion points within the same compartment, this can be overlooked.
Materials Needed:
Supplies to prepare your patient:
Sterile drapes/towels
Chlorhexidine or other topical antiseptic
Gauze 4 by 4s
Local anesthetic with needle and syringe
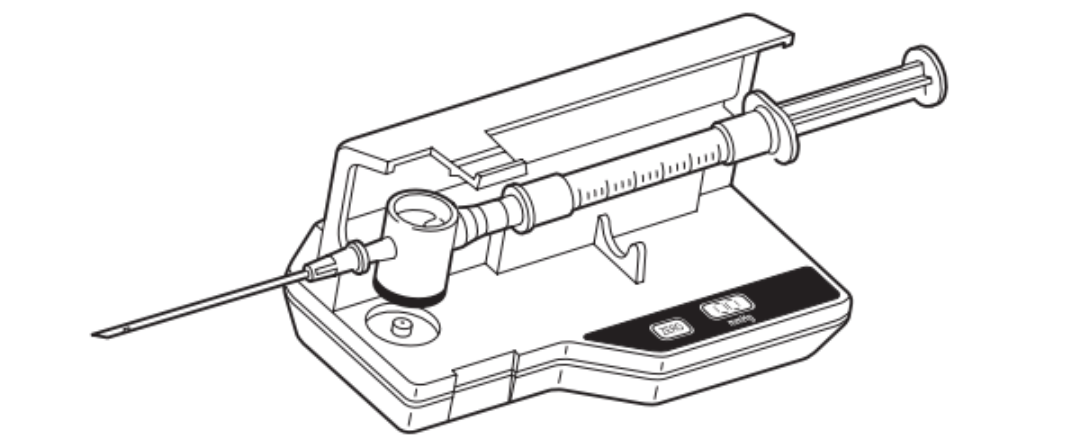
Supplies to measure compartment pressures (should all come in one prepackaged kit):
Pressure monitor unit
Side-ported needle
Prefilled syringe
Diaphragm
Relative Anatomy and Key Positioning:
The compartments of the forearm and lower leg are the most common sites of compartment syndrome; however, all compartments of the body can be affected including the fingers and abdominal wall.
In order to maximize the accuracy of our diagnosis of compartment syndrome, it is important to obtain the highest compartment measurement. There are different insertion considerations based on the mechanism of injury and whether a fracture is present. If a fracture is present, the needle should be inserted in the compartment at the level of the fracture site, with additional measurements approximately 5 cm above and below the fracture site. If no fracture is present or known, insertion at the site in the compartment of maximal tightness can be assessed or by the following “highest yield sites” based on the respective compartment.
Figure 1: Recommended insertion sites at the level of mid calf (A) and mid forearm (B)
Table 1: Needle Insertion Sites for the Compartments of the Leg
Table 2: Needle Insertion Sites for the Compartments of the Forearm
Studies have found that the position of the affected limb during the procedure can drastically affect the measurements. Flexing the muscles of the desired compartments at distal joints, whether actively or passively, is associated with increased and therefore inaccurate compartment pressure measurements. Therefore, it is important that patients are positioned with the limb in question at heart level in a neutral, relaxed-resting position.
Performing the Procedure:
Follow sterile procedure- clean and drape the affected compartment
Inject local anesthetic to anesthetize the area
Turn the manometer unit on. “ _ _” should display for five seconds then disappear- it should be ready to use now
Remove contents from the disposable pouch
Place needle firmly on tapered diaphragm stem
Remove cap of pre-filled syringe and screw onto the opposite side of the diaphragm chamber
Open cover of manometer and place chamber in the well with the black half of the diaphragm down
Snap manometer cover closed
Hold needle at 45 degrees above horizontal, slowly injecting fluid into diaphragm to release the air
Approximate the intended angle of insertion into the skin. Press the “ZERO” button to calibrate. It will read “00” when complete.
Insert needle into body compartment; inject approximately 0.3 cc saline to equilibrate with interstitial fluids
Read pressure
For additional measurements, repeat Steps 10-12.
Figure 2: Steps 5-6
Figure 3: Step 7
Figure 4: Step 10
Interpreting Your Results
The classic teaching is that a manometer pressure reading of over 30 mmHg is suggestive of compartment syndrome and warrants an emergency orthopedic or general surgery consultation for possible fasciotomy. However, a “delta pressure” of greater than 30 may be more accurate according to some studies. A delta pressure is obtained by subtracting the compartment pressure from the measured diastolic blood pressure. For patients who have elevated pressures but not yet diagnostic of compartment syndrome, serial measurements of compartment pressures can help trend and more closely monitor the situation.
High Yield Points
It’s important to have a low threshold for measuring compartment pressure in any one you suspect with compartment syndrome. That low threshold should also be extended to trending elevated, but not diagnostic, compartment pressures to ensure resolution.
Positioning and proper technique are key to accurate measurements–have the patient maintain a neutral, relaxed position and remember your MSK anatomy
No matter what method of compartment pressure measurement or result interpretation, remember the number “30” and alert your general surgery or orthopedic colleagues early, if you suspect compartment syndrome.
References:
Chapter 74. compartment pressure measurement. Reichman E.F.(Ed.), (2013). Emergency Medicine Procedures, 2e. McGraw Hill. https://accessemergencymedicine.mhmedical.com/content.aspx?bookid=683§ionid=45343715
C2Dx. (2021). STIC Instruction Guide. Schoolcraft, MI. Retrieved January 9, 2023, from https://c2dx.co/products/stic-pressure-monitor/#:~:text=STIC%20Intra%2DCompartmental%20Pressure%20Monitor&text=Formerly%20made%20by%20Stryker%20and,product%20you%20can%20rely%20on.
Ostermayer, D. (n.d.). Compartment Pressure Measurement - wikem. Compartment Pressure Measurement. Retrieved December 31, 2022, from https://www.wikem.org/wiki/Compartment_pressure_measurement
Torlincasi AM, Lopez RA, Waseem M. Acute Compartment Syndrome. [Updated 2022 Aug 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448124/
Tsintzas, D., Ghosh, S., Maffulli, N., King, J. B., & Padhiar, N. (2009). Ayak bileği pozisyonunun bacakta kompartman içi basinca etkisi [The effect of ankle position on intracompartmental pressures of the leg]. Acta orthopaedica et traumatologica turcica, 43(1), 42–48. https://doi.org/10.3944/AOTT.2009.042
Wheeless, C. R. (n.d.). Compartment syndrome : Wheeless' textbook of orthopaedics. Wheeless' Textbook of Orthopaedics. Retrieved December 31, 2022, from https://www.wheelessonline.com/muscles-tendons/compartment-syndrome/
Expert Commentary:
Dr Kubacki provided a great detailed step-by-step description of a procedure often intimidating to the Emergency Physician due to the infrequency this presentation; yet acute compartment syndrome (ACS) is a can’t miss diagnosis!
With regards to the 6 P’s of ACS, it must be emphasized the limitations of physical exam in assessing for ACS. Be especially aware of obtunded patients (i.e. from trauma or intoxication) who cannot verbalize symptoms, and that deeper compartments (i.e. thigh) may appear normal externally. An open fracture does not necessarily decompress the compartment and does not lower the risk for ACS. The swelling of ACS should be tense, almost woodlike. Many times we ask for orthopedic assessment and they are less concerned than we are because they will say the swelling seems soft. Also, don’t expect many of the the P’s to be present in any case. If so, there is likely already an advanced ACS. The key is to make the diagnosis before muscle dies!
The only contraindication I’d like to add is that when there is an obvious ACS, measuring compartment pressures can be skipped and the patient can go directly for fasciotomy. Here’s a helpful algorithm:
As mentioned by Dr Kubacki, the most useful number is not the absolute compartment pressure, it is the perfusion pressure, or ∆P, the Diastolic Blood Pressure minus the measured Compartment Pressure (∆P = DBP – ICP). ∆P <30 has been shown to be far more accurate for diagnosing ACS than absolute compartment pressure > 30.
For the procedure itself, here are some pitfalls:
- Not zeroing the manometer
- Depressing syringe plunger too quickly → transient falsely elevated reading
- Obstruction of needle with plug of tissue if syringe plunger pulled back
- Excessive deep infiltration of anesthetic → falsely elevated reading
Measurements are best obtained at the level of the heart.
For more information about checking compartment pressures, see this funny and informative video by NUEM alums Mike Macias and John Sarwark: https://vimeo.com/125208992
Matt Levine, MD
Emergency Medicine Physician, Northwestern Memorial Hospital
Associate Professor, Feinberg School of Medicine
How To Cite This Post:
[Peer-Reviewed, Web Publication] Kubacki, M. Moses, J. (2025, May 13). Compartment Pressure Measurement: Using the Stryker Method [NUEM Blog. Expert Commentary by Levine, M]. Retrieved from http://www.nuemblog.com/blog/compartment pressure measurement
Other Posts You May Enjoy