Written by: Maren Leibowitz, MD (NUEM ‘23) Edited by: Matt McCauley, MD (NUEM ‘21) Expert Commentary by: Seth Trueger, MD, MPH
Expert Commentary
Thank you both for your excellent overview of ketamine analgesia. For me, the biggest thing is recognizing it is just not a big deal, and the biggest challenge is people's hesitancy to use it because it seems like a bigger deal than it is.
The main principles I highlight:
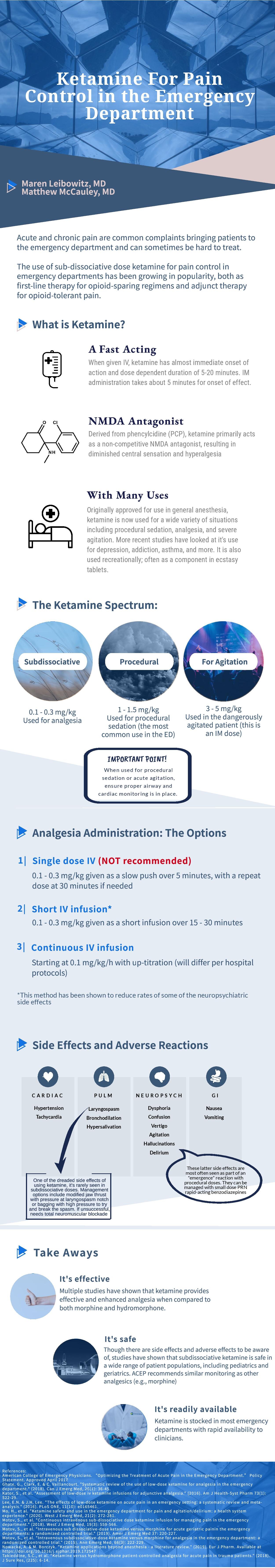
It's not hard, basically just give 0.1-0.3 mg/kg (20 mg is a good dose for most people).
The key is to give it in a small bag of saline, eg just mix it in 100ml and hang wide open (over about 20 min). This was demonstrated nicely in by Motov and colleagues (https://pubmed.ncbi.nlm.nih.gov/28283340/) and also resonates with my experience with patients.
This slow infusion minimizes (but does not eliminate) dysphoria/"feeling of unreality" some people get, and a slow hand push just does not do the trick. I also aim for 0.2mg/kg as rounding up can get people in the K-hole which is no fun (this is probably the only exception to my general rule of always use more, not less, anesthesia)
Ideally it's nice to do that dose as a bolus and then the same dose as a drip (eg 20mg over 20 min, followed by 20 mg per hour) but many EDs are unable to do that.
The easy way I think about it: a single does essentially replaces a dose of IV morphine- it does not require any more monitoring or have any increased risk of resp depression etc over morphine; ACEP, SEMPA & ENA have a statement on this. (https://www.acep.org/patient-care/policy-statements/sub-dissociative-dose-ketamine-for-analgesia/) It's just simply not sedation or dissociation (hence the term "sub-dissociative") and I have gotten in the habit of calling it "ketamine analgesia."
Perhaps the biggest downside is that for really severe pain, it works well but sometimes only as it's actively dripping in.
The situations I think about using ketamine analgesia are severe pain with contraindications to opioids (eg a patient with a fracture with a history of OUD who does not want opioids) or patients with severe pain where high doses of opioids are not sufficiently helping (eg malignant fractures, severe burns).
Theoretically we could use SDK all the time but there's a chicken/egg problem: we don't use it much, so people aren't very comfortable (plus some other various institutional/historical discomfort with ketamine in some sectors); also, realistically it doesn't last as long as IV opioids. Ideally I would probably use bolus + drip frequently if there weren't barriers.
Dr. Seth Trueger, MD
Assistant Professor of Emergency Medicine
Northwestern Memorial Hospital
How To Cite This Post:
[Peer-Reviewed, Web Publication] Leibowitz, M. McMauley, D. (2021, March 29.) Ketamine Pain Control. [NUEM Blog. Expert Commentary by Trueger, S]. Retrieved from http://www.nuemblog.com/blog/ketamine-pain-control.