Written by: Matt McCauley MD (PGY-3) Edited by: Jacob Stelter, MD (NUEM ‘19) Expert commentary by: Katie Wolfe, MD
Airway management of pediatric patients is a reasonable source of anxiety for the emergency physician. Children are intubated three to six times less often than adult emergency department patients [1]. Hence, it stands to reason that EP experience with mechanically ventilated children can be scarce [2] . Additionally, evidence driven practice in pediatric mechanical ventilation is limited and practice patterns vary between institutions and providers. These unknowns can make the prospect of managing these patients even more intimidating [3]. However, pediatric ventilator management is largely driven by data extrapolated from adults, which should come as a relief to the EP [4]. By keeping in mind small differences in pediatric physiology and keeping the consulting intensivist (and Broselow Tape) close at hand, an EP can effectively initiate mechanical ventilation in the smallest and most anxiety-provoking patients.
Getting Help
Like the Fat Man said in House of God: “[Disposition] comes first.” The intubated child is bound for a pediatric ICU and hopefully the accepting pediatric intensivist is already aware of any intubated patient and can be a great deal of help and support as you work together to make your patient safe for transfer upstairs or across town. Although the use of a Broselow tape and other height based methods of estimating body weight for drug dosing is fraught with error 5, the Broselow’s color coding allows for quick estimation of ideal body weight (IBW) that is required to calculate ideal tidal volumes.
Choosing a Mode
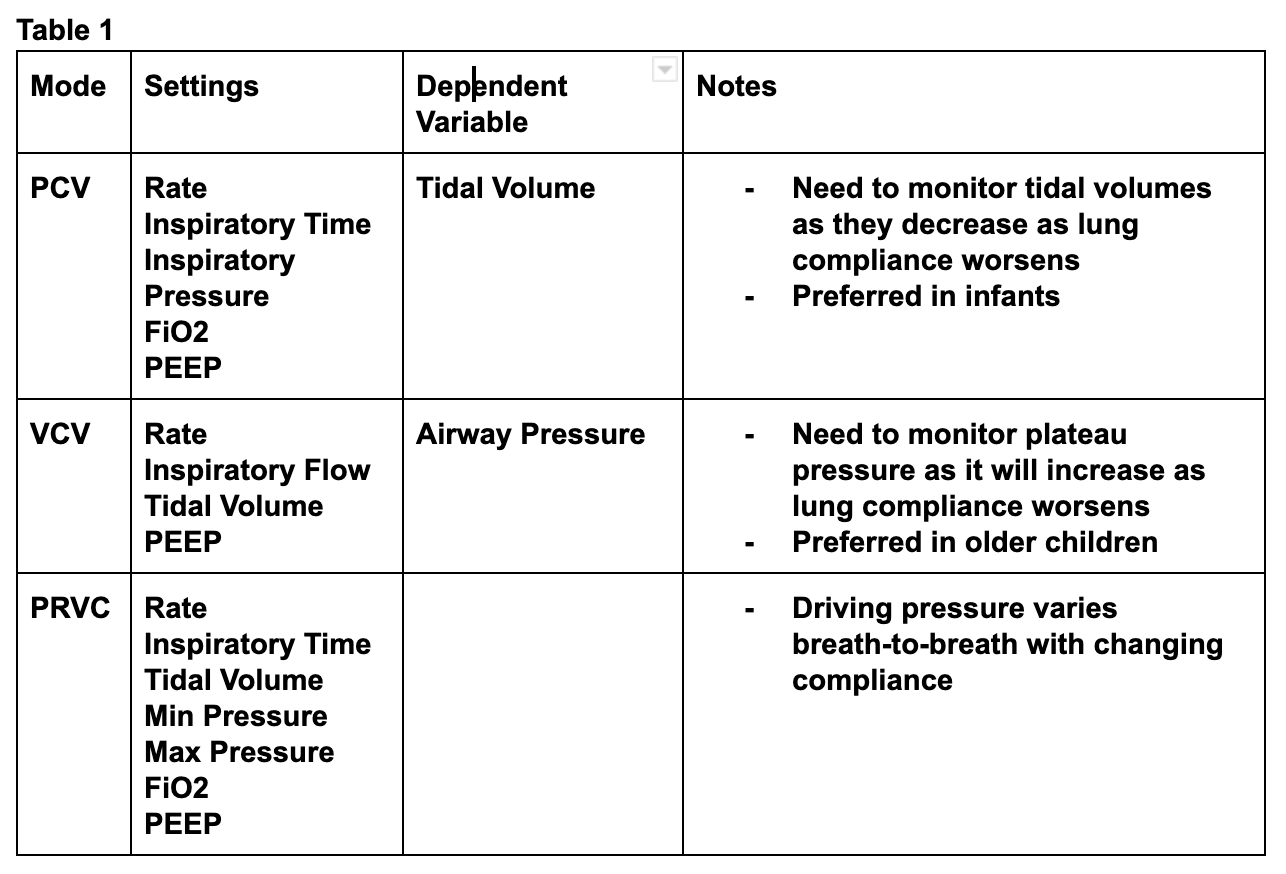
As mentioned, practice patterns related to pediatric ventilator management vary greatly [3]. The most commonly used modes for emergency pediatric ventilation include pressure assist control ventilation (PCV), volume control ventilation (VCV), and pressure regulated volume control ventilation (PRVC) [2]. PCV is typically favored in neonates and infants while volume modes are preferred in larger children [2]. When utilizing PCV, the provider sets the, inspiratory rate, inspiratory time, and inspiratory pressure meaning that the delivered tidal volume is dependent on the lung compliance of the patient [6]. This means that worsening compliance results in low tidal volumes. (Table 1)
Vt = Compliance x Delta Pressure
In contrast, VCV ventilation requires that the physician set the inspiratory rate, inspiratory flow rate, tidal volume, and PEEP. The ventilator delivers a fixed flow of air until the desired tidal volume is reached. This means that worsening compliance results in higher airway pressures (Table 1) [1]. The final commonly used mode for ventilating pediatric lungs is PRVC which, rather than requiring a set inspiratory flow rate like most volume controlled modes, utilizes a set inspiratory time, a targeted tidal volume, and a range of allowed pressures. With each breath the ventilator delivers a decelerating breath over the set time at an inspiratory pressure within the allowed range. If the resulting tidal volume is too high, the next breath is delivered with less pressure, if the volume falls short of the targeted tidal volume, the next breath is delivered with more pressure (Table 1) [6].
Finally, synchronized intermittent mandatory ventilation (SIMV) is often added to the above modes in pediatric ventilation. In SIMV, any time the patient initiates breaths within the set respiratory rate, a pressure supported breath (usually at 5-10 mmHg) is given rather than the full volume or pressure controlled breath. Pediatric patients are more likely than their adult counterparts to over-breathe the set respiratory rate, putting them at risk of breath stacking from large volume breaths. SIMV can help to mitigate this risk [2]. Despite all this complexity, there is a paucity of good evidence for or against any particular mode for ventilation the critically ill child [4]. This should reassure the EP to choose their most familiar ventilator mode in conjunction with their intensivist.
Choosing Age-Appropriate settings
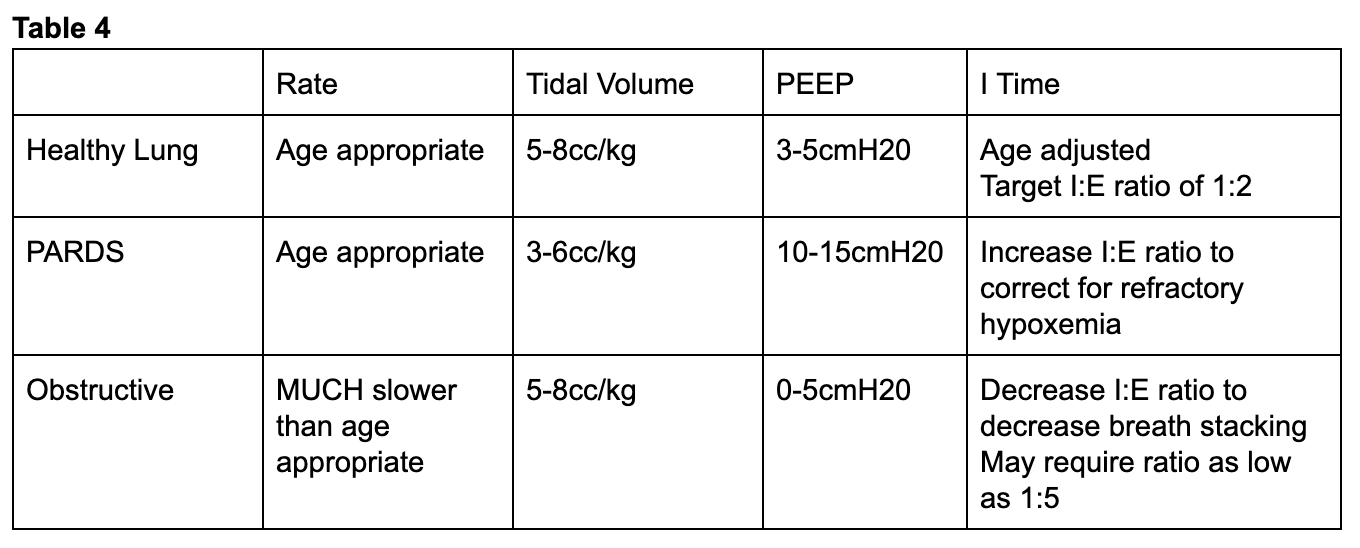
Since pediatric respiratory rates vary wildly from adults, one should take the patient’s age into account when initiating mechanical ventilation (table 2) . With the exception of children with obstructive pathophysiology, the physician should attempt to match the patient’s pre-intubation minute ventilation [2]. Tidal volume goals for pediatric patients do not vary much from adults with most data being extrapolated from adult studies [4] and large trials have been unable to establish as safe threshold for tidal volume [8]. The Pediatric Acute Lung Injury Consensus Conference (PALICC) recommends targeting 5-8cc/kg of ideal body weight (IBW) for most children either by setting a tidal volume in VCV or altering driving pressures for pressure controlled modes to target tidal volumes in this range for most patients [9]. Just as in adult patients, the intubating physician can set initial FiO2 at 100% to overcome hypoxia caused by peri-intubation apnea and then quickly down titrate targeting a SpO2 of 92-97% [9] .
If ventilating pediatric patients with pressure controlled ventilation, initially inspiratory times can be found on the Broselow or in a PALS manual 10 (table 3). If a volume controlled mode of ventilation is desired, inspiratory flow can be titrated to achieve a inspiratory to expiratory time ratio of 1:2 [2]. After initial setup, arterial blood gas analysis, continuous end-tidal CO2 measurement, and a chest X ray to evaluate tube positioning are just as critical here as they are in the adult patient.
Ventilating the Child with Refractory Hypoxemia
While most pediatric patients will be relatively straightforward to ventilate, the patient intubated for infectious pathologies like pneumonia or bronchiolitis is at risk for ARDS and should be approached with lung-protective ventilation strategies in mind. Victims of drowning are similarly at risk and fall under the category of patients requiring lung-protective settings [11]. There is no pediatric equivalent for the ARDSnet trial [12] so adult data has been extrapolated to be applied to pediatric patients [3] making this familiar territory for the adult emergency physician.
While most children will tolerate levels of PEEP between 3-5cmH204, PALICC recommends that children at risk of ARDS receive moderately elevated levels of PEEP between 10-15cmH2O with an SPO2 goal between 88-92% for kids requiring PEEP more than 10mmH2O [9]. In order to assess the extent of lung injury, an inspiratory hold maneuver can be used to determine lung compliance which is typically 1.5-3.0/cmH2O/kg for an infant [2]. If the EP notes decreased compliance, tidal volumes closer to 3-6cc/kg should be targeted [9]. If these measures fail to improve oxygenation, inspiratory time can be increased in order to target an inspiratory to expiratory ratio closer to 1:2. With the exception of children with elevated intracranial pressure (ICP), congenital heart disease, or pulmonary hypertension, permissive hypercapnea is acceptable as long as the pH remains > 7.2 [4].
Ventilating the Child with Obstructive Physiology
Endotracheal intubation of the asthmatic child is thankfully a rare event but one that portends to a high mortality [13]. At baseline, children exhibit higher airway resistance than their adult counterparts [2] and the even higher airway resistance in asthmatic patients creates high levels of intrinsic PEEP while increases the risk of breath stacking and pneumothorax [14]. If the patient’s respiratory rate is too high, lungs will remain progressively inflated at end expiration. This increases intra-thoracic pressure thereby decreasing preload and precipitating cardiovascular collapse. The level of this intrinsic PEEP can be assessed with an expiratory hold maneuver (Figure 1). To do this, the ventilator occludes the expiratory port at the end of exhalation allowing the alveolar and airway pressures to equilibrate. The total pressure at this moment minus the set PEEP on the ventilator represents the intrinsic PEEP [7]. More simply, a flow/time curve that fails to return to baseline prior to the onset of inspiration may signal to the EP that there may be high levels of intrinsic PEEP 2. (Figure 2)
To counteract this, asthmatics and other patients with obstructive physiology will need respiratory rates far below median age values. In one series of asthmatic children aged as young as nine months, rates as low as 8-12 breaths per minute were used [15]. In order to further facilitate full expiration, the I:E ratio should be increased to target values as low as 1:4-5 [15]. High levels of PEEP are typically not required in these patients and use of low to zero PEEP has been documented [14]. Hypercapnea should be expected and is allowable in these patients [14].
Prolonged mechanical ventilation of the pediatric patient exhibits far more complexities than this blog post covers and is beyond the scope of most emergency medicine practice. However, by relying on evidence driven practice for adult intubated patients with close guidance from a pediatric intensivist and pediatric resuscitation reference, the initial steps and safe monitoring of the intubated child are well within the abilities of the emergency physician.
Expert Commentary
Thank you for this concise summary of mechanical ventilation in children. As noted, while this is an infrequent occurrence, the initial management of a ventilated child is incredibly important.
In choosing initial ventilator settings, the key is decision and reassessment. Most modes of ventilation will work in most children. However, careful attention to what support you’re providing your patient with and what the results of that support are, is vital. Personally, I like using PRVC mode because it adjusts support in children with changing lung compliance without a lot of manipulation required by the physician. But, in any mode of ventilation you can make adjustments as you note changes in compliance. In pressure mode, watch your tidal volumes and in volume control or PRVC, monitor your peak pressures (along with your saturations and end tidal) to see if you’re achieving your goals. Use of SIMV versus AC modes of ventilation are important in the weaning phase of ventilation but less important as you’re initiating mechanical ventilation as the patient is typically neuromuscularly blocked. I also want to emphasize the importance of weaning supplemental oxygen as soon as possible in order to understand the adequacy of your support from an oxygenation and ventilation standpoint. Hypoxemia is bad but so is hyperoxia and masking hypoventilation.
While the research in pediatric ARDS is not as robust as in adults, there is a growing body of literature describing epidemiology and current practice.[1] Current management strategies continue to be extrapolated from adult data- including lung protective strategies of permissive hypoxemia and hypercarbia (tidal volumes 3-6 cc/kg, saturations >92% in mild pARDS and >88% in severe pARDS, pH > 7.2 with exceptions for specific populations including those with pulmonary hypertension).[2] Restrictive fluid strategies (after initial resuscitation) and adequate sedation are recommended. There is ongoing research regarding the use of HFOV and prone positioning in pARDS but this is outside the scope of emergency department care.
The intubated asthmatic remains a source of anxiety among many pediatric intensivists. Key takeaways are low respiratory rate to allow for full exhalation and prevent air trapping and matching intrinsic PEEP. Permissive hypercapnia is appropriate in these patients and their CO2 should be measured by blood gas; recognizing that there is a significant amount of dead space and end tidal may be falsely reassuring/low. When intubating patient with obstructive physiology, it’s also important to ensure adequate preload and have a high suspicion for pneumothorax if they decompensate. Utilizing ketamine for sedation can be useful in these patients and has the advantages of bronchodilation and not significantly suppressing their respiratory drive, allowing them to participate in setting their inspiratory/expiratory times.
Final thought: don’t hesitate to ask for help- from the pediatric intensivists in house or over the phone- we are happy to collaborate!
References:
Khemani RG, Smith L, Lopez-Fernandez YM, et al. Paediatric acute respiratory distress syndrome incidence and epidemiology (PARDIE): an international, observational study. Lancet Respir Med. 2019 Feb;7(2):115-128. doi: 10.1016/S2213-2600(18)30344-8. Epub 2018 Oct 22.
Orloff KE, Turner DA, Rehder KJ. The Current State of Pediatric Acute Respiratory Distress Syndrome. Pediatr Allergy Immunol Pulmonol. 2019 Jun 1; 32(2): 35–44. doi: 10.1089/ped.2019.0999. Epub 2019 Jun 17.
Dr. Katie Wolfe, MD
Attending Physician
Pediatric Critical Care
Ann & Robert H. Lurie Children's Hospital of Chicago
Instructor of Pediatrics (Critical Care)
Northwestern University Feinberg School of Medicine
How To Cite This Post
[Peer-Reviewed, Web Publication] McCauley, M. Stelter, J. (2020, Feb 3). Initiating Emergency Department Mechanical Ventilation in the Pediatric Patient. [NUEM Blog. Expert Commentary by Wolfe, K]. Retrieved from http://www.nuemblog.com/blog/ped-mech-vent.
Other Posts You Might Enjoy…
References
Losek J.D., Olson L.R., Dobson J.V., et al: Tracheal intubation practice and maintaining skill competency: survey of pediatric emergency department directors. Pediatr Emerg Care 2008; 24: pp. 294-299
Pacheco, G. S., Mendelson, J., & Gaspers, M. (2018). Pediatric Ventilator Management in the Emergency Department. Emergency Medicine Clinics of North America, 36(2), 401–413. https://doi.org/10.1016/j.emc.2017.12.008
Rimensberger, Peter C., Ira M. Cheifetz, and Martin C. J. Kneyber. “The Top Ten Unknowns in Paediatric Mechanical Ventilation.” Intensive Care Medicine 44, no. 3 (2018): 366–70. https://doi.org/10.1007/s00134-017-4847-4
Kneyber, Martin C. J., Daniele de Luca, Edoardo Calderini, Pierre-Henri Jarreau, Etienne Javouhey, Jesus Lopez-Herce, Jürg Hammer, et al. “Recommendations for Mechanical Ventilation of Critically Ill Children from the Paediatric Mechanical Ventilation Consensus Conference (PEMVECC).” Intensive Care Medicine 43, no. 12 (December 2017): 1764–80. https://doi.org/10.1007/s00134-017-4920-z.
Wells et al. The accuracy of the Broselow tape as a weight estimation tool and a drug-dosing guide – A systematic review and meta-analysis. Resuscitation. 2017 Dec;121:9-33.
Singer, BD. Corbridge, TC. "Pressure modes of invasive mechanical ventilation" Southern Medical Journal" 104, no. 10 October 2011, pp 701-709
Singer, BD. Corbridge, TC. "Basic Mecahnical Ventilation" Southern Medical Journal" 102, no. 12 December 2009 , pp pp 1238-1245
de Jager P, Burgerhof JG, van Heerde M, et al: Tidal volume and mortality in mechanically ventilated children: A systematic review and meta-analysis of observational studies*. Crit Care Med 2014; 42:2461–2472
Rimensberger PC, Cheifetz IM. Ventilatory support in children with pediatric acute respiratory distress syndrome: proceedings from the pediatric acute lung injury consensus conference. Pediatr Crit Care Med.(2015) 16(5 Suppl. 1):S51–60. 10.1097
Chameides L, Samson RA, Schexnayder SM, Hazinski MF (Eds).Pediatric Advanced Life Support Provider Manual, , American Heart Association, Dallas 2012.
Semple-Hess, J., & Campwala, R. (2014). Pediatric submersion injuries: emergency care and resuscitation. Pediatric Emergency Medicine Practice, 11(6), 1–21
Kneyber, Martin C. J. “Mechanical Ventilation for Pediatric Acute Respiratory Distress Syndrome: Few Known Knowns, Many Unknown Unknowns.” Pediatric Critical Care Medicine: A Journal of the Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies 17, no. 10 (2016): 1000–1001.
Rampa S, Allareddy V, Asad R, et al. Outcomes of invasive mechanical ventilation in children and adolescents hospitalized due to status asthmaticus in United States: a population based study. J Asthma 2015; 52:423.
Rubin, Bruce K., and Vladimir Pohanka. “Beyond the Guidelines: Fatal and near-Fatal Asthma.” Paediatric Respiratory Reviews 13, no. 2 (June 2012): 106–11. https://doi.org/10.1016/j.prrv.2011.05.003.
Cox, R. G., G. A. Barker, and D. J. Bohn. “Efficacy, Results, and Complications of Mechanical Ventilation in Children with Status Asthmaticus.” Pediatric Pulmonology 11, no. 2 (1991): 120–26