Introduction
I’ve been suffering in that waiting room for hours!
That worthless tech stabbed me with a needle ten times!!
If you don’t give what I want right now, I am going to hurt someone!!!
Every emergency physician can recall a time when they hear these words or similar phrases echoing throughout the Emergency Department (ED). As a patient becomes increasingly agitated, nearby staff and visitors become distracted, and ultimately concerned about everyone’s safety. Emergency Physicians can help restore the calm amidst the chaos by recognizing subtle clues and intervening early.
According to the Bureau of Labor Statistics, those who work in the healthcare sector had three times the rate of illness and injury from violence compared to all private industries [1]. In a survey of emergency medicine residents, 65.6% reported an experience of physical violence by a patient, 96.6% reported verbal harassment from a patient, and 52.1% reported sexual harassment by a patient. Often these patients were under the influence of drugs or alcohol, had a psychiatric disease, or an organic cause of their agitation, such as dementia [2]. In Australian emergency departments, 3 of every 1000 ED visits are associated with an episode of violence or acute behavioral disturbance [3].
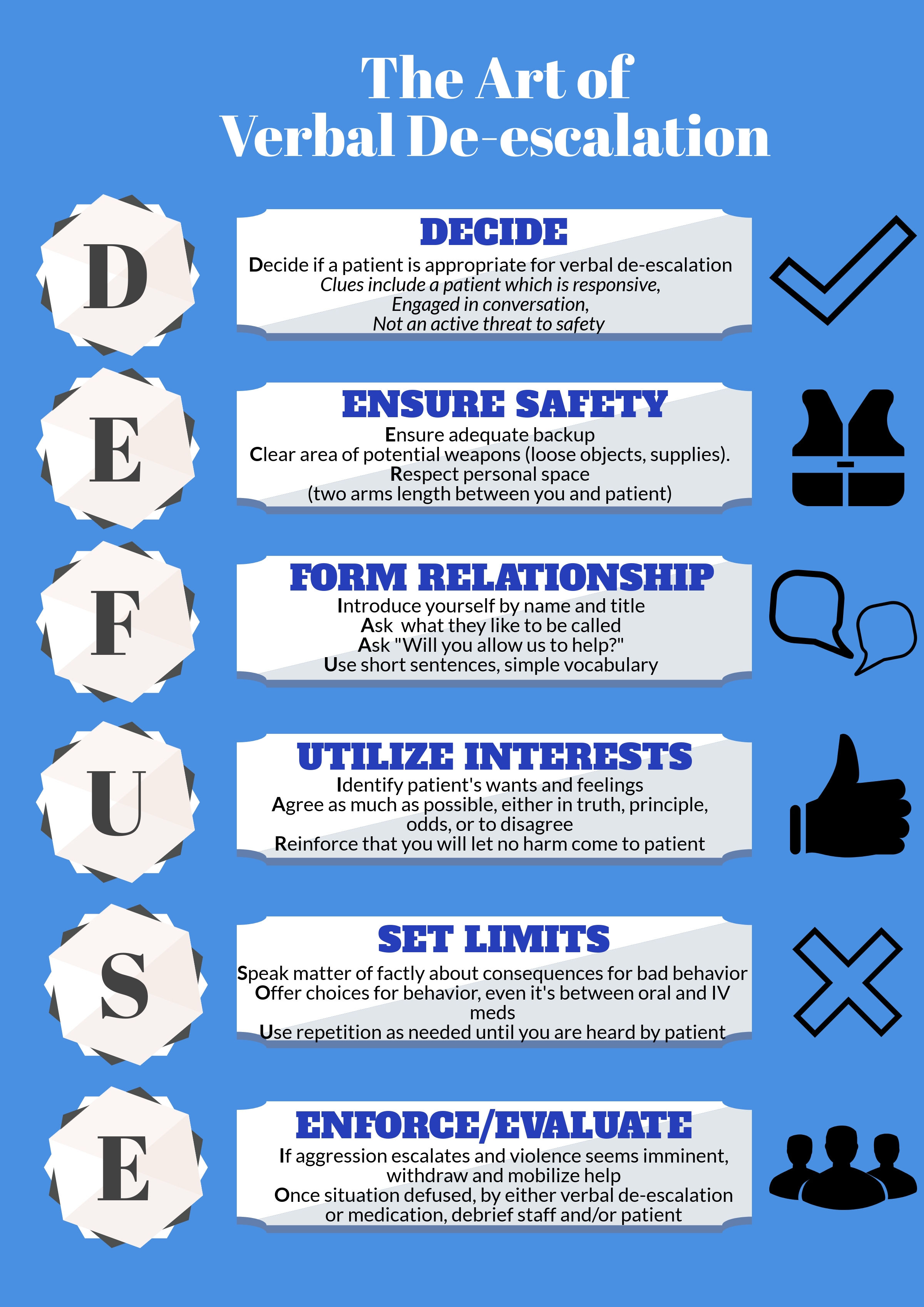
When violence by a patient is imminent or has already occurred, the patient requires immediate restraint by either chemical or physical means [4]. ACEP guidelines for patient restraints supports the careful and appropriate use of restraints or seclusion if “careful assessment establishes that the patient is a danger to self or others by virtue of a medical or psychiatric condition and when verbal de-escalation is not successful [5].” Verbal “de-escalation techniques aim to stop the ascension of aggression to violence, and the use of physically restrictive practices, via a range of psychosocial techniques [6],” and should be tried before one simply grabs “5 and 2.”
Clinical Approach to Agitation
How do you determine which patients would benefit from verbal de-escalation?
Look for the agitated patient, the one who has an angry demeanor, using loud and aggressive speech, seems tense and is grasping their bed rails or clenching their fists, the one who is pacing or fidgeting [4]. These patients are in the pre-violent stage, and may have the potential to be successfully talked down. If a patient has already engaged in violent acts, it is too late to intervene with verbal de-escalation methods.
What principles should be used to assist with verbal de-escalation of the agitated patient?
In 2012 the American Association for Emergency Psychiatry offered a consensus statement on verbal de-escalation and created ten key domains to guide care of agitated patients. These domains offer a great framework for how to approach the agitated patient before the situation escalates [7].
Domain 1: Respect the patient’s and your personal space. First and foremost in any patient encounter, especially one with an agitated patient, is your safety. Aim to keep at least 2 arms lengths distance between you and the patient. This offers you room for your own personal safety, and is seen as non-confrontational and non-threatening in the eyes of the patient. Ensure that both you and the patient have an unobstructed pathway to the exits and that you do not stand in the way of the patient’s path to leaving the room.
Domain 2: Do not be provocative. The majority of our interpersonal interactions is communicated not by the words we say, but how we say them. Our body language is crucial and we must be mindful of it when attempting to calm a patient. Keep your hands visible and at ease, bend your knees slightly, avoid excessive direct eye contact and approach your patient from an angle instead of head-on. These positions convey a non-threatening demeanor.
Domain 3: Establish verbal contact. The first person to interact with the patient should be the one who leads the verbal de-escalation. Introduce yourself and tell the patient your role and orient them to their surroundings. Then, ask the patient what they would like to be called. This gives the patient the impression that you believe he or she is important and has some control over the situation.
Domain 4: Be concise and caring. Use short sentences and simple vocabulary to get your point across. Give your patients time to process what you have said and to respond before continuing. You should be prepared to repeat your message multiple times until your patient understands.
Domain 5: Identify wants and feelings. In order to provide empathetic care, you must understand your patient’s perspective. Listen carefully to what your patient says to pick up clues and respond to their desires. One tactic is to say “I really need to know what you expected when you came to the ED today. Even if I can’t provide it, I would like to know so that we can work on it together.”
Domain 6: Listen closely to what the patient is saying. This is closely related to Domain 5. Practice closed loop communication, repeat what the patient has told you to ensure you have understood them correctly.
Domain 7: Agree, or agree to disagree. Look for something that you can agree with in what the patient is saying. “I agree, waiting can be frustrating” or “Yes, I understand that the nurse has stuck you three times.” However, if you can’t find something to agree with the patient about, do not lie - agree to disagree.
Domain 8: Lay down the law and set clear limits. Draw a line which the patient must not cross. Let him or her know that harming himself or others is unacceptable and will result in specific consequences (seclusion, arrest, prosecution). This should not be portrayed as a threat, but rather be conveyed in a respectful manner. You can preface it with “Your behavior is making our staff uncomfortable and that makes it difficult for us to help you.”
Domain 9: Coach the patient on how to stay in control. Give the patient tactics they can use to help de-escalate the situation. “If you sit down we can discuss why you are here.”
Domain 10: Be optimistic and provide hope that the patient will be able to get to a favorable outcome. “I don’t want you to stay here longer than you need to. Let’s work together to help you get out of here feeling better.” Be sure to debrief with the patient and staff after the de-escalation, so that there is a strategy in place if this were to happen again.
Other strategies include recruiting the patient’s friends and family to help and to employ the three Fs technique - feel, felt, found [8]. “I understand that you feel X. Others in the same situation have felt that way to. Most have found that doing Y can help [4].”
Think of verbal de-escalation as a procedure just like intubations or central lines - with practice, comes mastery. Rehearse what you plan to say, and do mental run-throughs of de-escalations. Watch and learn from others who do this well. The English Modified De-Escalating Aggressive Behaviour Scale (EMDABS) is a validated tool you can use to assess your performance during de-escalations [9].
Summary
Unfortunately, physical and chemical restraint of the severely agitated patient is sometimes needed to protect ED staff, visitors, and the patient themselves. [10,11]. But by recognizing subtle signs of agitation early, we can often utilize effective verbal-de-escalation techniques to create safety for everyone!
Check out our infographic for an easy to use mnemonic which summaries key points.




































































































































![[6]](https://images.squarespace-cdn.com/content/v1/549b0d5fe4b031a76584e558/1543862052562-UD9VZ6Q6971A7Y2S1L2P/Picture1.png)
![Panel A displaying a crusted lesion in the ear of a patient with RHS. Panel B highlights the CN VII palsy that can be seen in RHS.[9]](https://images.squarespace-cdn.com/content/v1/549b0d5fe4b031a76584e558/1543862567359-HTGAWD5SRS937LJDEX9I/Picture2.png)
![[12]](https://images.squarespace-cdn.com/content/v1/549b0d5fe4b031a76584e558/1543862655499-KYEV6LWKYDYHX5KCPEYI/Picture3.png)